Dr. Phil Zeltzman’s Blog
6 ways to prepare for your pet’s surgery

Surgery is a big deal, and we want you to be fully prepared and comfortable with the plan.
Here are 6 simple steps to be ready for the big day.
1. Blood work
We always recommend pre-anesthetic blood work to make anesthesia and surgery as safe as possible. Seemingly healthy pets on the outside can have serious problems on the inside. They could cause complications during anesthesia and surgery.
Pre-anesthetic blood work will confirm:
- Liver and kidney health
- Red and white blood cell count
- Enough platelets for proper clotting
- Enough protein to ensure healing and clotting
- Balanced electrolytes, which can affect the stability of the heart under anesthesia.
Discovery of a small imbalance will allow us to adjust drugs or IV fluids before, during, and after your pet’s anesthesia and surgery.
Unless it’s an emergency and we don’t have the luxury of time, detection of a serious problem may lead us to postpone surgery until the pet’s condition is stable.
This can happen with high liver values, which could justify an ultrasound to make sure we’re not missing something important.
2. Medications
We will let you know which medications to continue or stop before anesthesia. And we’ll tell you when to resume them.
Other drugs are given to reduce stress and the risk of vomiting around anesthesia time.
An added benefit is that it will allow us to give less anesthesia to your pet.
3. Rest
Anesthesia and surgery can take a toll on the body, so let your pet chill the day before surgery.
It’s just like a human: provide plenty of rest the day before surgery.
Plan on a relaxed day, full of TLC.

4. Instructions
Follow the instructions you are given verbally and in writing.
Failing to do that could potentially prevent your pet from having safe anesthesia and surgery.
Following them will increase the chances of success.
Also make sure you fully understand postop instructions, i.e. what you will need to do as far as confinement, feeding, medications, supplements, activity, physical therapy, wound care, leash walks, etc.
5. Preparation
Prepare your home for your pet’s return.
We will explain in great detail how to confine your pet, which type of flooring is ideal, which toys are allowed, how to feed your pet etc.
Depending on the type of surgery, we may also recommend:
- getting a harness for your dog
- changing the litter for your cat
- using soft food only
Again, this all depends on the surgery, and we will help you get fully prepared.

6. Feeding
An empty stomach is important to decrease the risk of vomiting before, during, and after anesthesia.
With a few exceptions, we recommend taking food away at 8 pm the night before surgery.
Water however is important to prevent your pet from getting dehydrated.
So water is allowed until you leave home, the morning of surgery.
If you ever have a question about your pet’s care, before or after surgery, never hesitate to call.
Our only goal is a happy outcome for you and your pet.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Common questions about arthritis

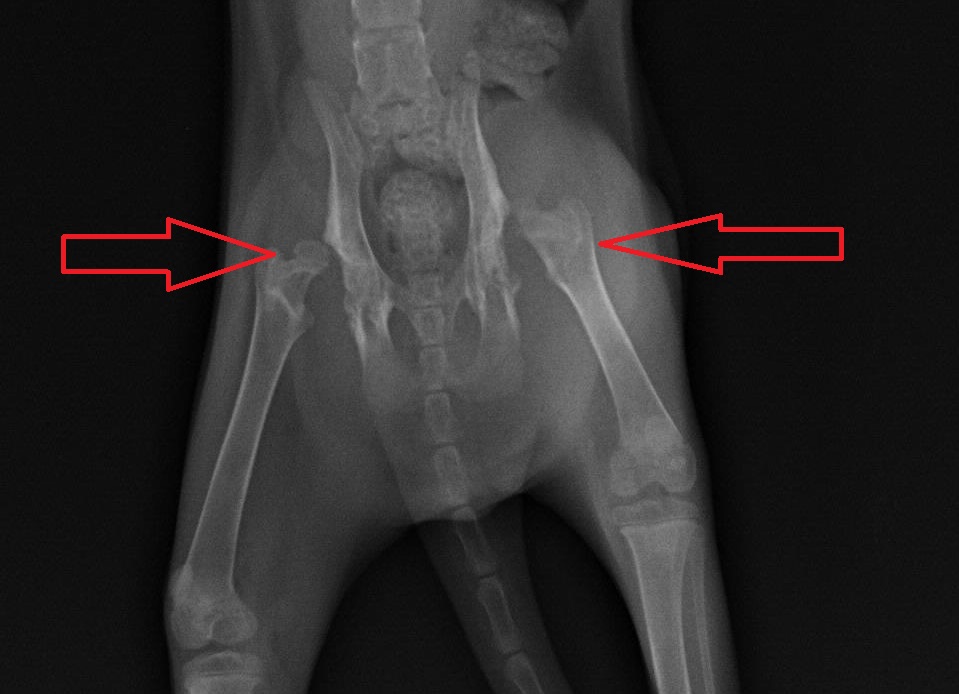
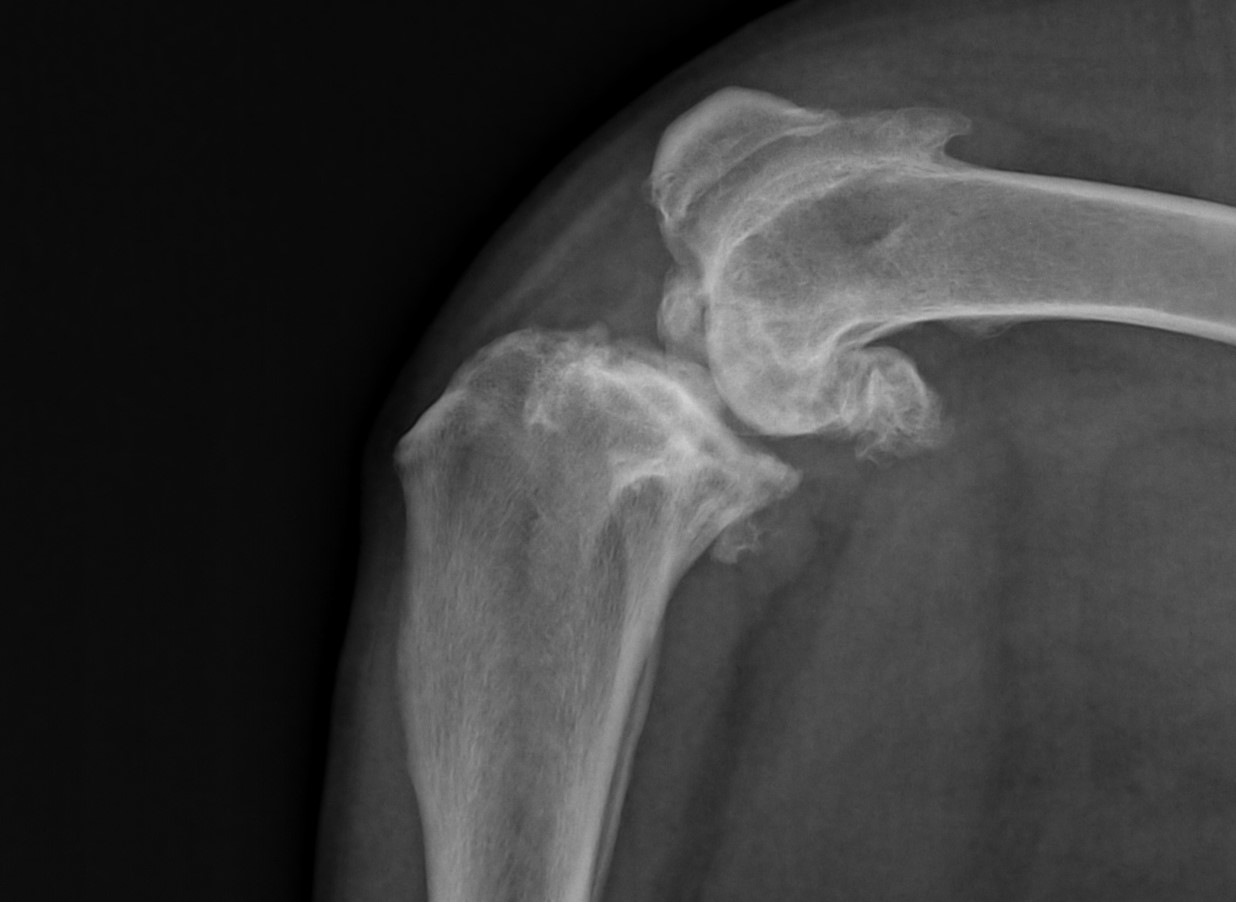
Last June, we answered the very common question: “How can my pet have arthritis so young?”
(here is the link to that blog: https://www.drphilzeltzman.com/blog/how-can-my-pet-have-arthritis-so-young/).
Today, let’s answer more very common questions related to arthritis.
1. Can arthritis be cured?
There is no cure for arthritis, in pets or in people.
In most cases, for example in the case of Amber the Lab with a torn ACL and Sweetie with dislocated kneecaps, who were featured in the blog mentioned above, we cannot get rid of arthritis once it has developed.
In Tank’s case, we “removed” the arthritis by removing the ball part of the joint during surgery.
In most cases, all we can do is slow down the progression and manage the signs. Don’t believe the hype, Dr Google or the advertising.
There is no way to prevent arthritis and there is no magic cure once it starts.
That said, there are several options to support the joint, slow down the progression and reduce inflammation (irritation). Beyond surgery, or after surgery, we can give joint or arthritis supplements. They most commonly include glucosamine (with chondroitin) and fish oil (omega-3 fatty acids).
We know that arthritis gets worse with time, so time is of the essence.
We can’t fix the arthritis, but the sooner we address the issue, the better off your pet will be long-term.
The pain can be addressed by a number of great and safe pain medications, including anti-inflammatory drugs.
2. Will you remove the arthritis during surgery?
We cannot just magically remove arthritis while we are in surgery.
Technically speaking, we could remove some of the bone spurs we see, but not all of them. Whether with traditional “open” surgery or with arthroscopy (a camera in the joint), we simply don’t have access to all of the bone spurs.
Even if we could remove them, they would come back. So removing them doesn’t really serve a purpose.
The only exception is in the case of FHO surgery of the hip. Refer to these 2 recent blogs:
- the one mentioned above, where we talk about Tank.
- a blog dedicated to hip dysplasia: www.drphilzeltzman.com/blog/what-to-do-about-hip-dysplasia
3. How do I know my pet has arthritis?
Arthritis is often assumed, without any proof, especially in older pets.
One simple way to prove a pet has arthritis is with a simple X-ray.
Common changes include:
- decrease in mobility
- limping, lameness, favoring a leg
- difficulty jumping
- new limitations during physical activity
- sleeping or napping more
- reluctance to go on long walks
- not grooming as much (especially cats)
- difficulty going up or downstairs
- stiffness from getting up after resting for a while
- seemingly aging prematurely.

Bottom line: the sooner you notify your family vet or your surgeon, the more options we might have to help your pet.
4. What else can be done to help my pet with arthritis?
You can find more information in this blog:
www.drphilzeltzman.com/blog/10-ways-to-help-a-pet-with-arthritis
Don’t give up. There is help out there!
If you would like to learn more about how your pet can have safe surgery and anesthesia, contact us through www.DrPhilZeltzman.com.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
www.DrPhilZeltzman.com

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What Complications Can Happen at Home After Anesthesia? (Part 4)

Even though a pet may have gone through surgery and anesthesia very smoothly, they can still have a few complications after they leave the hospital.
In part 1, we discussed breathing complications.
In part 2, we discussed cardio-vascular complications.
In part 3, we discussed other complications that can happen during anesthesia.
Today, let’s discuss other complications that can happen AFTER anesthesia.
Let’s go over the most common ones – which can also happen in people.
1. Constipation
Many pets will not have a bowel movement for the first few days after anesthesia and surgery. There are several reasons for that:
- Your pet has been fasted prior to surgery
- Your pet may not have eaten well during the hospital stay or the first few days at home
- Anesthesia drugs and pain medications may slow down your pet’s transit
If your pet does not have a bowel movement within 4-5 days after returning home, your vet or surgeon will often suggest a stool softener.
Please always follow a vet’s advice, because some “human” stool softeners are toxic to pets, mostly in cats.
Also note that some pets will occasionally have the opposite reaction and will have diarrhea, possibly due to stress.

2. Lethargy, nausea, poor appetite
All these can happen after anesthesia.
Your pet simply doesn’t feel well after anesthesia and/or surgery.
The drugs do get out of the body very quickly (some within minutes, most within hours).
Still, it may take a few days to get over anesthesia, just like in a person.

3. Dysphoria
This can certainly happen in cats, but it’s more obvious in dogs who wake up from surgery.
They are often discombobulated.
They have no idea what happened to them.
They may not know who you are and where they are.
They’re spacey or groggy or loopy, while the full effects of anesthesia wear off.
They pace. They can’t sit still. They can’t rest.
They can’t “seem to get comfortable.”
They won’t lie down for hours at a stretch.
If you’ve ever had anesthesia, you likely felt the same way.
You may also have seen videos of kids or adults waking up from anesthesia, after dentistry or surgery, and they say the weirdest or funniest things – which they don’t even remember later.
Since dogs don’t understand what’s happening, it causes anxiety.
And they don’t know how to express that, except through whining.
While it’s stressful to any pet lover, the good news is that it should go away after a good night’s sleep – rarely longer than that.
If you doubt it, let me give you a classic example. If we only sedate a dog (not even full anesthesia) to take X-rays or change a bandage or trim their nails, and reverse the drugs, they may experience dysphoria.
We haven’t done anything painful, yet they cry like they’re in severe pain.
Why is that? Well, it’s exactly for the reasons explained above. It’s not pain. It’s dysphoria. They’ll get over it, so please be patient with your pup!
Bottom line: This type of crying should stop or at least improve when you sit next to your dog, or you call his or her name.
Thankfully, all of the above complications are most often short-lived.
If not, you should definitely call your vet or surgeon to discuss the situation.
There is no guarantee with any anesthesia.
Yet these days, the risks of severe complications are small, and most complications resolve quickly.
The secret is to have good monitoring equipment, and above all, experienced anesthesia nurses.
Every patient we anesthetize has a dedicated anesthesia nurse, whose only job is to keep her patient safe.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What other complications can happen during anesthesia? (part 3)

The healthiest patient can run into complications during anesthesia.
In part 1, we discussed breathing complications.
In part 2, we discussed cardio-vascular complications.
Today, let’s discuss other complications that can happen during anesthesia.
1. Hypothermia
This word means that the body temperature is too low. We do all kinds of things to prevent hypothermia before, during and after anesthesia: heating blankets, forced-air warm blankets, warm IV fluids etc.
If the temperature were still too low, we would find even more solutions to increase it back to normal.
2. Hyperthermia
This is the opposite of hypothermia, so this means that the body temperature is too high.
It can occur because of an unpredictable reaction to anesthesia drugs, which is thankfully extremely rare.
Less common, sometimes we use so many devices to increase a patient’s temp, that it goes a bit too high. This is especially true in small patients. We would then stop 1 or 2 options until the temp is back to normal.
3. Bleeding
Bleeding is an inevitable occurrence during any surgery.
The surgeon’s job is to minimize it.
In some rare cases, the bleeding is so significant (for example, a large tumor that bleeds excessively), that a blood transfusion is necessary.
4. Regurgitation
Under anesthesia, the stomach relaxes, and stomach fluid can easily go “up.”
This is a bit similar to acid reflux in people.
Worst case scenario, a few days after anesthesia, it can lead to aspiration pneumonia as explained below.

5. Aspiration
Under anesthesia, patients can’t control their swallowing reflex, so it is possible that fluid from the stomach can end up in the throat.
From there, the fluid can go down the trachea (wind pipe) and into the lungs.
This is called aspiration.
Once in the lungs, fluid or food can cause a type of pneumonia called aspiration pneumonia.
To reduce this risk, we recommend fasting the patient after dinner time, the night before surgery. In at-risk breeds, such as dogs with a flat face (Bulldogs, Pugs, Bostons…), we routinely give 2 anti-vomiting drugs and an antacid.
The same drugs can be given before specific surgeries, such as abdominal surgery, in any breed.
Thankfully, this is a rare occurrence.
As you can see, the risks of these complications are small, and most complications can be solved quickly.
The key is to have good monitoring equipment, and above all, experienced anesthesia nurses.
Every patient we anesthetize has a dedicated anesthesia nurse, whose only job is to keep her patient safe.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What cardio-vascular complications can happen during anesthesia? (part 2)

This is part 2 of our anesthesia complications blog series. You can read part 1 here.
The bad news: Every anesthesia carries some risk.
The good news: most complications are minor, and quickly and easily fixable.
Let’s go over some cardio-vascular anesthesia complications.
1. Bradycardia
Bradycardia is a fancy word that means that the heart rate is too low.
Common causes include:
- The anesthesia is too deep. The simple solution is lower the amount of anesthesia gas.
- The body temperature is too low. This is something we fight from start to finish.
- Electrolyte abnormalities. Most commonly, it is related to potassium being too high in the blood. This can happen in pets with a blockage that prevents them from urinating. We try to correct that before anesthesia even starts.
- Morphine-like drugs. That’s a common side-effect. If the heart rate is too low, we can use drugs to increase it.
2. Tachycardia
Tachycardia is the opposite of bradycardia, so it means that the heart rate is too fast.
The most common causes include:
- The anesthesia is too low. The simple solution is to give a bit more.
- Pain. We would then give even more pain medications than we typically provide.
- Some diseases, such as a tumor in the adrenal gland. This would be temporary, until the tumor is removed, and we can use drugs to lower the heart rate if needed.
3. Hypotension
Hypotension means that the blood pressure is too low, just like in some people.
The most common causes include:
- Severe bleeding. The solution would be to give more IV fluids or possibly a blood transfusion.
- Cardio-vascular diseases. Hopefully, this is something we know ahead of time, and can treat with meds before anesthesia starts. We sometimes use different drugs for anesthesia. We are also less generous with IV fluids so we don’t overload the heart.
- The anesthesia is too deep. We would then provide less anesthesia gas.
- Some drugs. We can give IV fluids or drugs that can correct that.
- Some conditions. For example, mast cell tumors in the skin can release a substance that causes the blood pressure to drop. We routinely use drugs before anesthesia to prevent this from happening.

4. Hypertension
Hypertension is the opposite of hypotension, so it means that the blood pressure is too high, just like in some people. The most common causes include:
- The anesthesia is too light. So we would simply give more anesthesia drugs.
- Some diseases. For example, a type of tumor of the adrenal gland (pheochromocytoma) can release a substance that causes the blood pressure to spike. There are drugs we can use to lower the blood pressure.
5. Arrhythmias
Arrhythmia is a fancy word that means that there are abnormal or extra heartbeats.
The most common example is extra heartbeats during “bloat” (twisted stomach) or spleen surgery.
This usually resolves eventually with drugs and time.
Fortunately, the risks of severe complications are small, and most complications can be solved quickly.
The key is to have good monitoring equipment, and above all, experienced anesthesia nurses.
Every patient we anesthetize has a dedicated anesthesia nurse whose only job is to keep her patient safe.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!

