Dr. Phil Zeltzman’s Blog
10 reasons to see a surgeon specialist

Before we start, I would like to point out a few important thoughts:
- A specialist is not a competitor of your family vet. Rather, the specialist should be considered as an extension of your primary care veterinarian, similarly to what happens in human medicine.
- The ideal situation is that your family vet and the specialist have a prior relationship. They may not have dinner once a week or be BFFs, but they should work well as a team and communicate well – for your benefit and your pet’s.
- It is important to remember that there are many family vets with considerable expertise in various areas despite not being “specialists.” Yet it is not possible that any one vet can be an expert in all areas.
- The only vets who can call themselves specialists, or “board-certified,” or “boarded” in short, are those who have gone through additional training beyond vet school (8 years): an internship (usually 1 year) and a residency (typically 3 years). Then, they must pass a very difficult exam. The only proof of all of that is extra letters after their name. For a surgeon, you should see DACVS or Dip. ACVS or Diplomate ACVS after their name.

That said, let’s go over my top 10 reasons to see a board-certified surgeon:
- A surgeon has extensive training. You tend to do well what you do often.
- A surgeon may have treated several patients like your pet. Surgeons naturally see more challenging cases because so many family vets refer to them.
- A surgeon has the specialized equipment needed. There are surgeries you simply cannot possibly do without special equipment.
- A surgeon can provide a second (or third) opinion.
- A surgeon tends to know the latest research and advances, because all they read is surgery journals and all they attend is surgery conferences.
- Some patients may need a high-risk or difficult surgery.
- Some patients may require specialized anesthesia because they are “high-risk”.
- A surgeon’s clinic might provide 24-hour care, which is extremely rare in family practice.
- A surgeon and their nurses offer comprehensive pain management through multiple modalities. For example, in my practice, we use 10 different ways to prevent and treat pain before, during and after a TPLO (a surgery to address a torn ACL).
- Performing a surgery is a technical act. Knowing how to prevent complications, or how to deal with them if they occur, is a whole different story.

Basically, you should see a specialist for your pet for the same reasons you would see a specialist for yourself for open heart surgery or joint surgery.
So if your pet needs surgery, have an open discussion with your family vet and decide if they can handle it, or if you should consider a surgeon specialist.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What surgeons secretly want you to know…

I asked some surgeon friends what they would tell you if they could sit down with you and have a casual chat around coffee… (tea is allowed).
You can learn a lot from their answers.
There is no sugar-coating here.
I will share their loving, nurturing, bluntly honest tips, then mention their names & locations below. If you ever need surgery for your pet, they are excellent surgeons you can trust.
GENERAL ADVICE
- Dogs are not small people. Cats are not small dogs. Medications used on one cannot always be used safely on the other. Some drugs, given to the wrong patient, can even be deadly.
- If you are not sure about what to do, or if you’re confused about something, or if you forgot what you were told, ASK. There are no stupid questions.
- Your pet may be chubbier than you think. That little bit of chub that you think is hiding under all that fur is more than you realize. It might be cute on a baby, but not on your dog. Thin and fit are essential to a long and healthy life.
- Dr Google is not your friend. A Google search does not replace the years of education and practice needed to become a veterinarian – or a surgeon.
- Don’t be mad at your vet when they give you advice, yet you choose to trust Dr Google or your breeder and things don’t turn out the way you want.
- The receptionists and nurses who support your vet are critical to the function of a pet hospital and the care of your pet. We can’t work without them. Be kind. Treat them with respect. We ALL have your pet’s best interest at heart. That’s the only reason we chose this profession.
- Spay your female pet before the first heat to virtually eliminate the risk of breast tumors. And it will help decrease or eliminate all kinds of bad or expensive diseases.
- Neuter your male dog during puppyhood. It will help decrease or eliminate all kinds of bad or expensive diseases.

AVOIDING COMPLICATIONS
- Surgeons are highly allergic to complications. So we design our postop instructions to minimize the risks to your pet. Our postop instructions are based on science and years of experience.
- Postop care is harder than you want and more important than you realize. We don’t make up recommendations for fun. Or to torture your pet. Or to torture you. They have a purpose and we need you to follow them to reach a happy outcome.
- Why is confinement so critical after a TPLO or a fracture repair? Because if something goes wrong because your pet escapes your care, or because you didn’t follow the rules, the damage could be FAR worse than where we started. And sometimes, the damage is beyond repair… and could require amputation.
- Just because a pet complains about something doesn’t mean that you shouldn’t do it. Just because they don’t like confinement, work, physical therapy or taking pills does it mean they shouldn’t do it. For the same reasons we make kids brush their teeth and take a shower!
Now… also use your judgement.
If your pet hates it when you apply cold or heat, then discontinue it and don’t force it.
If your pet truly hates it when you do physical therapy, then discontinue it, don’t force it, and call your surgeon to try to find out what might be going on.
- Confinement after surgery is not a punishment. It’s a necessity to allow proper healing.
- How does your surgeon choose the duration of confinement? It has to do with how long it takes to heal. In an adult, bone takes 2 months to heal. In a puppy or a kitten, it could take 6 weeks.
It has nothing to do with you or our personal preference. It has to do with Mother Nature.
WHO TO TRUST
- Being a surgeon is different from doing surgery. Many veterinarians do surgery. Very few of us are actually trained as surgeons. Going to a weekend course does not make you a surgeon. Ask tough questions. Do your homework.
- You often get what you pay for. Don’t choose the cheapest option. Then again, don’t believe that the most expensive option is the best one… Choose the best surgeon you can find, based on experience, results and reputation.
- Any surgeon you work with should be willing to answer those 3 simple questions:
– How many times have you performed this surgery?
– What results do YOU get?
– Would you do it on your own pet?
- Being a surgeon does not give us superhuman vision. And NOBODY can give you a diagnosis just by feeling a mass or by looking at it. We need to submit tissue samples to a pathologist to look under a microscope to know what it is. Or we need to take X-rays to see what’s going on inside. Guessing does not help you or your pet.
- The kid at the pet store doesn’t know anything about pet nutrition. Trust your vet.
- Your breeder does not have a veterinary degree. Trust your vet.
- 80% of supplements sold online and at pet stores are complete junk. Trust your vet.
TUMOR REMOVAL
- The first time is the best time. Having someone remove a mass only to find out they didn’t get it all is not a great idea. A second surgery means more expenses for you, more trauma for your pet, and no guarantee that we can get it all the second time around.
- “Just watch it” are the least favorite words of surgeons and oncologists (cancer specialists) alike. Getting cells or tissue samples from a mass to evaluate under a microscope can be the difference between life and death for your pet. Or skip the preop testing, and put the money toward surgery and postop testing.
- Don’t wait until masses are big enough that they bother YOU. Deal with them while they’re small and manageable. Surgery will be cheaper, less invasive and possibly less dangerous if the mass is small.

PETS AND PAIN
- Animals are very good at hiding pain. Remember, in the Wild, animals that show pain get eaten.
This means 2 things:
– Before surgery, pets will hide their signs and their pain until they just can’t take it anymore.
– After surgery, pain medication should be given as directed by your vet. Don’t stop early, thinking your pet is doing OK because they act normal. Pain meds also decrease inflammation and help rebuild muscles.
- Pets don’t become addicted to pain medications, including morphine-like drugs. Plus, they don’t have thumbs to open the pill bottles…
POSTOP CARE
- Dogs and cats feel better and act like they’re better LONG before they have actually healed. Don’t let those sad eyes trick you into shortening their convalescence period!
- Elizabethan collars (E collars) are used to deter your pet from licking, chewing, scratching or rubbing the incision. Most incision complications are due to self-trauma, ie licking or scratching. Despite the old wives’ tale that dog saliva helps with healing, the truth is that licking, chewing or scratching an incision can lead to skin irritation, infection, pain and prolonged healing if the incision falls apart. Not to mention more fees and more aggravation.
- Leave the E-collar on at ALL times. Your pet will be able to eat and drink and figure out how to get through that doorway eventually! Talk to your surgeon about which style is best for you and your pet’s particular condition.
- Yes, it is OK, and even preferred, for your dog to use the leg after TPLO surgery or a fracture repair. Exactly when they will start to use the leg is tough to predict, but rest assured that if they do use it, it’s because they can.
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified
SOURCES:
Thank you to my amazing colleagues for their generous contribution:
- Kathy Collins, board-certified surgeon at Veterinary Surgical Services in Rochester and Buffalo, NY.
- Jennifer Wardlaw, board-certified surgeon at Gateway Veterinary Surgery in Saint-Louis, MO.
- Mario Cabrera, surgeon at Cutting Edge Surgical Referrals in Miami, FL.
- Tony Kahn, board-certified surgeon at Anchor Veterinary Surgery in New York, NY.
- Tracy Nicole Frey, board-certified surgeon at SoftSurg in San Diego, CA.
- Jeremiah Moorer, board-certified surgeon at Trek Veterinary Surgery, in Denver, CO.
- I also contributed a few gentle & loving thoughts… Phil Zeltzman, board-certified surgeon in Bethlehem, PA & Harrisburg, PA.

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Jake, my biggest surgical & ethical challenge in 2022

Jake, an 11 year old Golden, had a long list of issues…
- A mass in his left anal sac, which was likely cancerous.
- A right-sided perineal hernia, because he was not neutered.
- An enlarged prostate, because he was not neutered.
He needed 4 separate surgeries to solve these issues:
- Removal of the anal sac mass.
- Repair of the perineal hernia.
- Abdominal surgery to deal with the prostate.
- A neuter.
That’s a lot for one older dog, and a long anesthesia.
That begged a critical question: was it safer to do everything under one anesthesia (and take a risk) or separate different surgeries under 2 separate anesthesia episodes (and take a risk)?
In other words, one very long anesthesia (possibly 2-3 hours) could be risky in an older dog. He could have a much longer recovery. Now, I’d be the first one to tell you that anesthesia is incredibly safe these days, but it makes sense that a longer anesthesia is riskier than a short anesthesia.
So the next question was: would 2 shorter anesthesia episodes, a few weeks apart, be safer?
And if we decided to separate the surgeries in 2 sessions, what should we do first and second?
I agonized over what to do.
I consulted with surgeon colleagues to brainstorm about the wisest approach.
It was a huge ethical & medical dilemma.
In the end, I decided not to gamble and perform 2 separate surgeries.
I had a long heart-to-heart with Jake’s owner. She understood the reasoning and was ready to get started.
Anesthesia 1:
We decided to perform everything on the “back end” during the first anesthesia.
- Right perineal hernia repair: a perineal hernia is a bizarre condition, most commonly found in non-castrated male dogs. The muscles that keep organs inside the belly become weaker. This can allow organs to slip through the pelvis and end up under the skin, on either side (or both) or the anus.
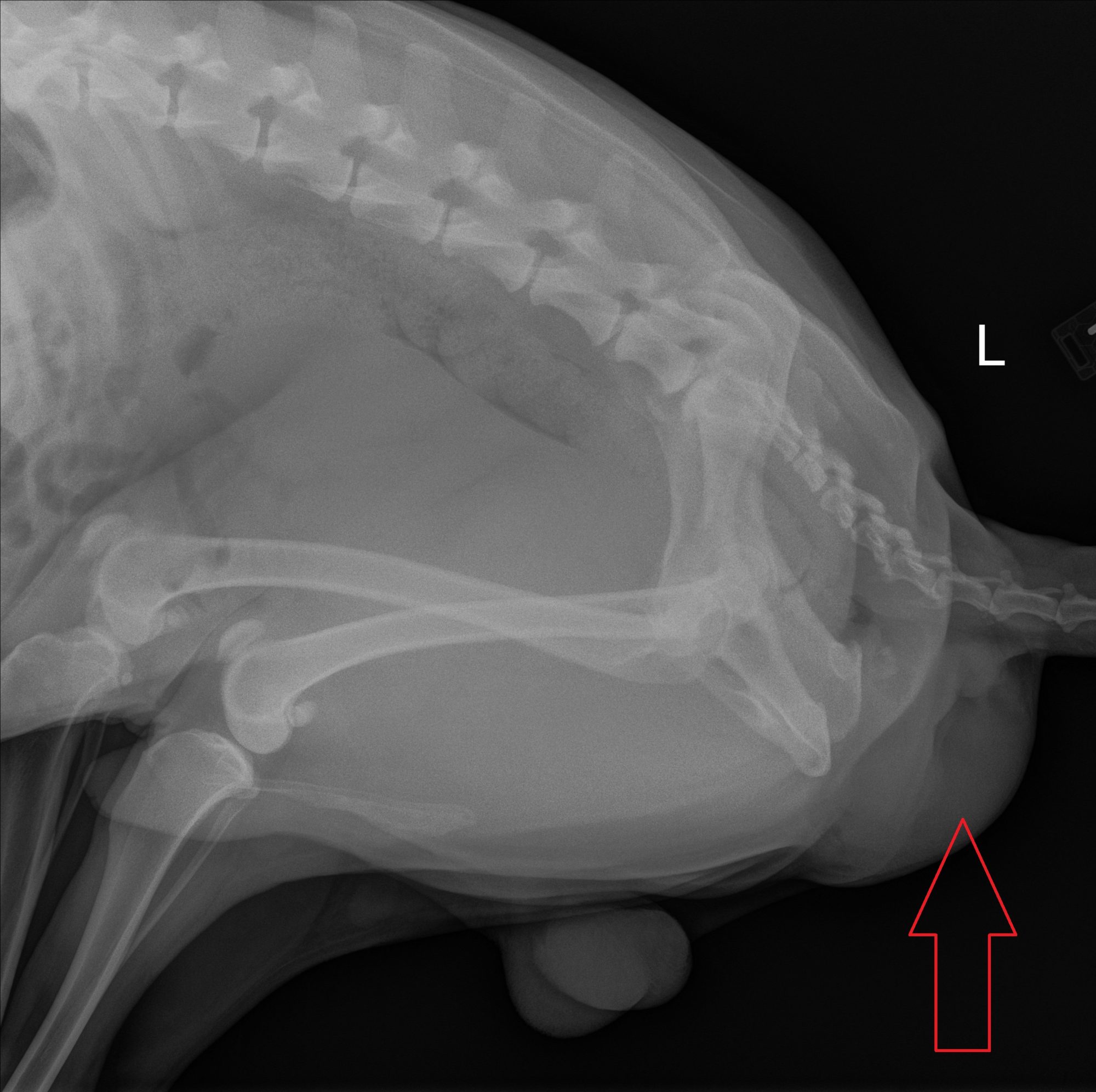
Below is a picture of the back end of another dog, Tommy, with a huge bulge on the right side of the anus. It contained the prostate & the bladder.
In other patients, the hernia can even contain intestines.

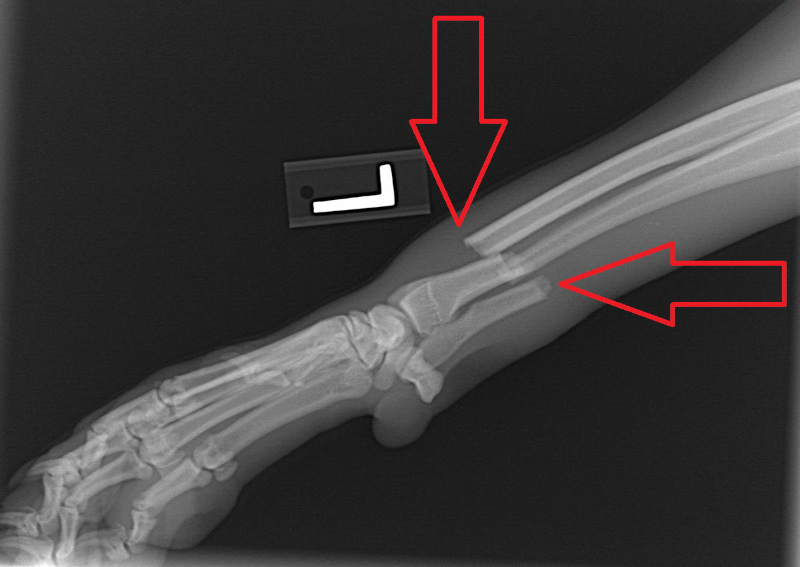
You can see Jake’s hernia in the X-ray below. The bulge in his back end is the hernia. In Jake’s case, it contained fat and a lot of fluid.
- Left anal sac mass: then we dealt with the tumor. It was tiny (2 mm, or less of a tenth of an inch), but most of the time, such masses are cancerous and aggressive. This was one of the reasons to perform the “back end” surgeries first: to get rid of presumed cancer ASAP. Sure enough, the biopsy came back as the classic cancer in an anal sac (adenocarcinoma). It was small enough that we got it all.
Jake has his family vet to thank for that. Not only did she find the tiny mass by doing a thorough exam (including a rectal exam), but she recommended surgery rather than procrastinating.
- Neuter: Then Jake was neutered. I also recommended removing his scrotum (the “sac”), for shall we say… cosmetic reasons…
Jake did great through anesthesia, and went home to recover over the following month.
Anesthesia 2:
One month later, Jake was back to normal and we performed the belly surgery to deal with the very large prostate found on ultrasound.
The prostate cannot be removed safely. We drained it by using a natural “drain” that lives in the belly, called the omentum. This thin membrane that floats in the belly is very rich in lymphatic vessels, and can drain pus and fluid from the prostate. This is called “omentalization.”
We also took biopsies of the prostate. The biopsy revealed that Jake’s condition was “benign prostatic hyperplasia,” along with multiple cysts. It can cause difficulty peeing, which is also the classic condition in older gentlemen…
In dogs, castration is the treatment of choice. The lack of testosterone causes the prostate to shrink over a few weeks.
This time again, Jake did great through anesthesia, and went home to recover over the following month.
Over 7 months after his first surgery, Jake is still doing great!
His owner was happy with the sequence of events, and with the end result: a happy, healthy, tail-wagging Golden!
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Toto can’t pee because of bladder stones!
Toto, an 8 year male terrier, had difficulty urinating. He was painful and struggled to pee, and not much urine came out despite his efforts.

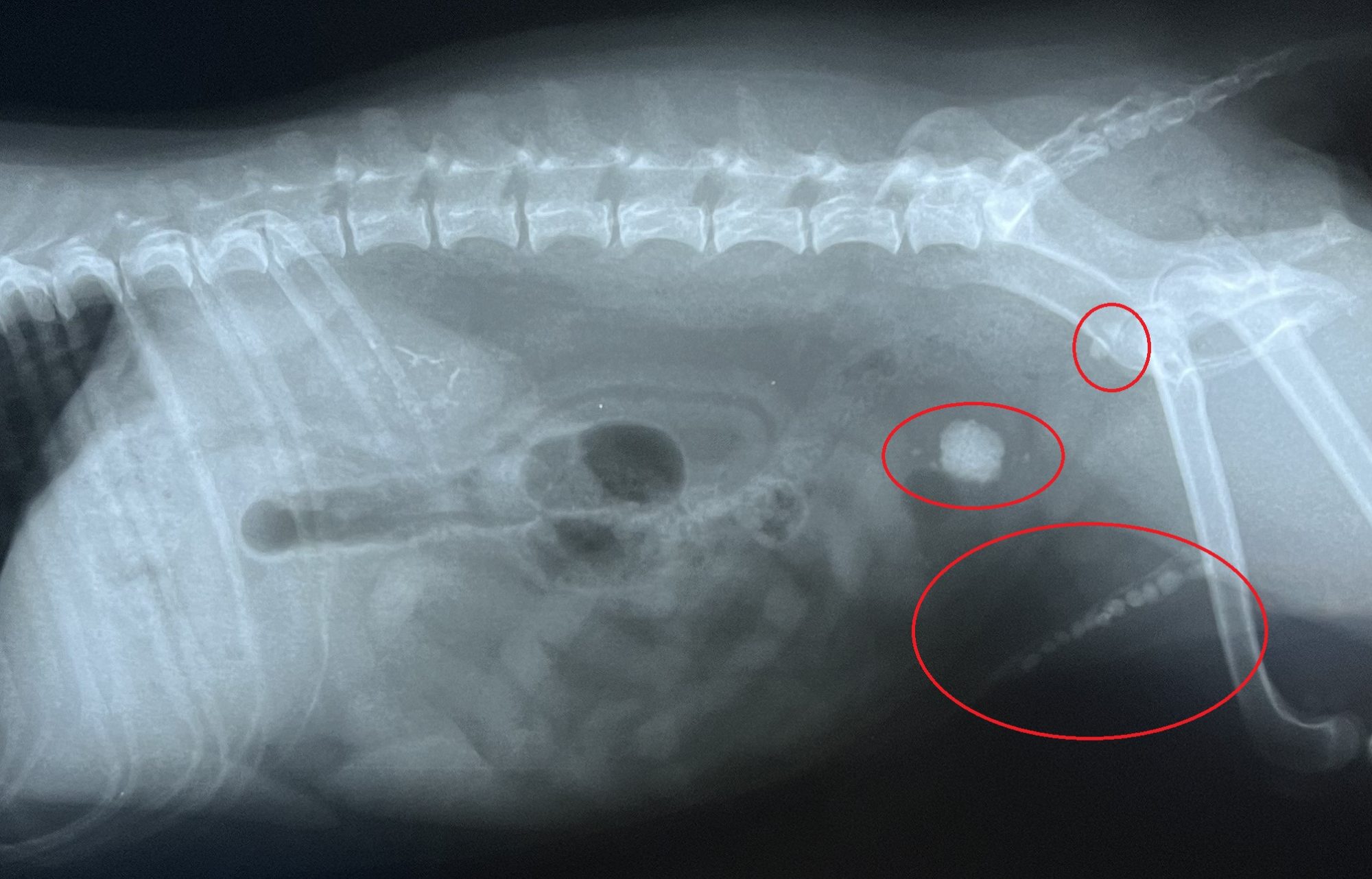
An exam and X-rays revealed that he had stones in the bladder. The blockage was caused by smaller stones that were formed in the bladder, then were small enough to go down into his urethra. The urethra is the tube that goes from the bladder to the penis. The small stones lined up in the urethra like a string of (deadly) pearls.
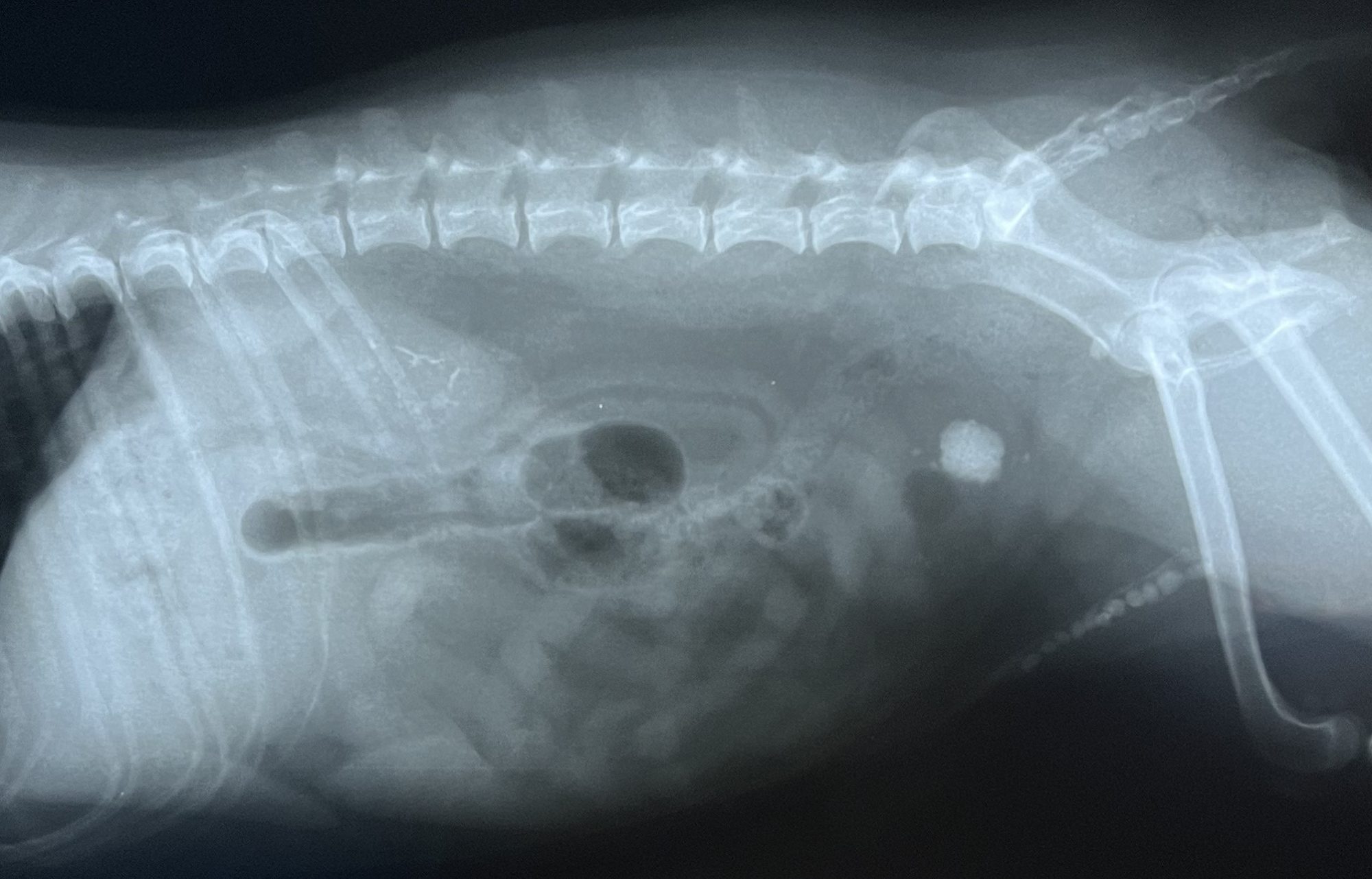
Can you spot all stones?
Here is the same X-ray with the bladder (2 ovals at the top) & urethral stones (oval at the bottom) circled.
The easy part was to perform bladder surgery (aka cystotomy) to remove the big stone and a few small ones.
Here is the big bladder stone:

The hard part was to push the tiny, spiky stones from the urethra back into the bladder, from which they can easily be removed.
If that doesn’t happen because the stones are literally stuck in the urethra, then a second surgery needs to be done to create a new, larger opening in the urethra (aka a urethrostomy). This can be done successfully, but we always try to avoid it.
Because I know that my readers and subscribers are sensitive souls, I can’t explain exactly how the stones are moved from the urethra into the bladder. Let’s just say that we use sterile saline under pressure. As a reminder though, the patient is under general anesthesia during surgery!
It was an amazing surgery. Initially, the stones didn’t bulge at all.
We kept pushing more and more sterile saline – nothing.
Then all of a sudden, 3 small stones came out.
After multiple other unsuccessful attempts, another 2 stones came out.
The whole team was watching and cheering as my nurse and I struggled to push these stubborn stones back into the bladder.
So we continued to fight for Toto.
Little by little, stone by stone, we managed to move all of the stones into the bladder.
Toto didn’t need a urethrostomy after all.
Surgery was a success!
Here are the small urethral stones:

Toto was eventually able to go home, where he had to rest very strictly for 3 weeks. He had to wear a plastic cone around his head to prevent him from licking the incision. He recovered smoothly and has been happily urinating ever since surgery. He was switched to a special food to try to prevent the stones from coming back.
A few weeks after surgery, the stone analysis results confirmed the suspicion of “calcium oxalate” stones, i.e. they were made of calcium. So Toto had to eat that special diet exclusively for the rest of his life.
Toto’s surgery was truly challenging. It took a lot of effort, but in the end, the fight was worth it.
I just checked on Toto. Four years after surgery, he’s still peeing like a champion!
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Never miss a blog by subscribing here: www.DrPhilZeltzman.com/blog
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Extreme makeover: Novakai and the cleft palate

“You should be prepared for this puppy to die.”
This is the terrifying advice Novakai’s owner was given.
Novakai, a cute 7 month old Pitbull, did have a big problem in her mouth.
A cleft palate divided the entire roof of her mouth in two halves.
This gap allowed food to go from her mouth into her nose.
PICTURES BELOW ARE GRAPHIC AND ARE NOT FOR THE FAINT OF HEART.
All of the pictures below show the inside of the roof of the mouth, with Novakai on her back.
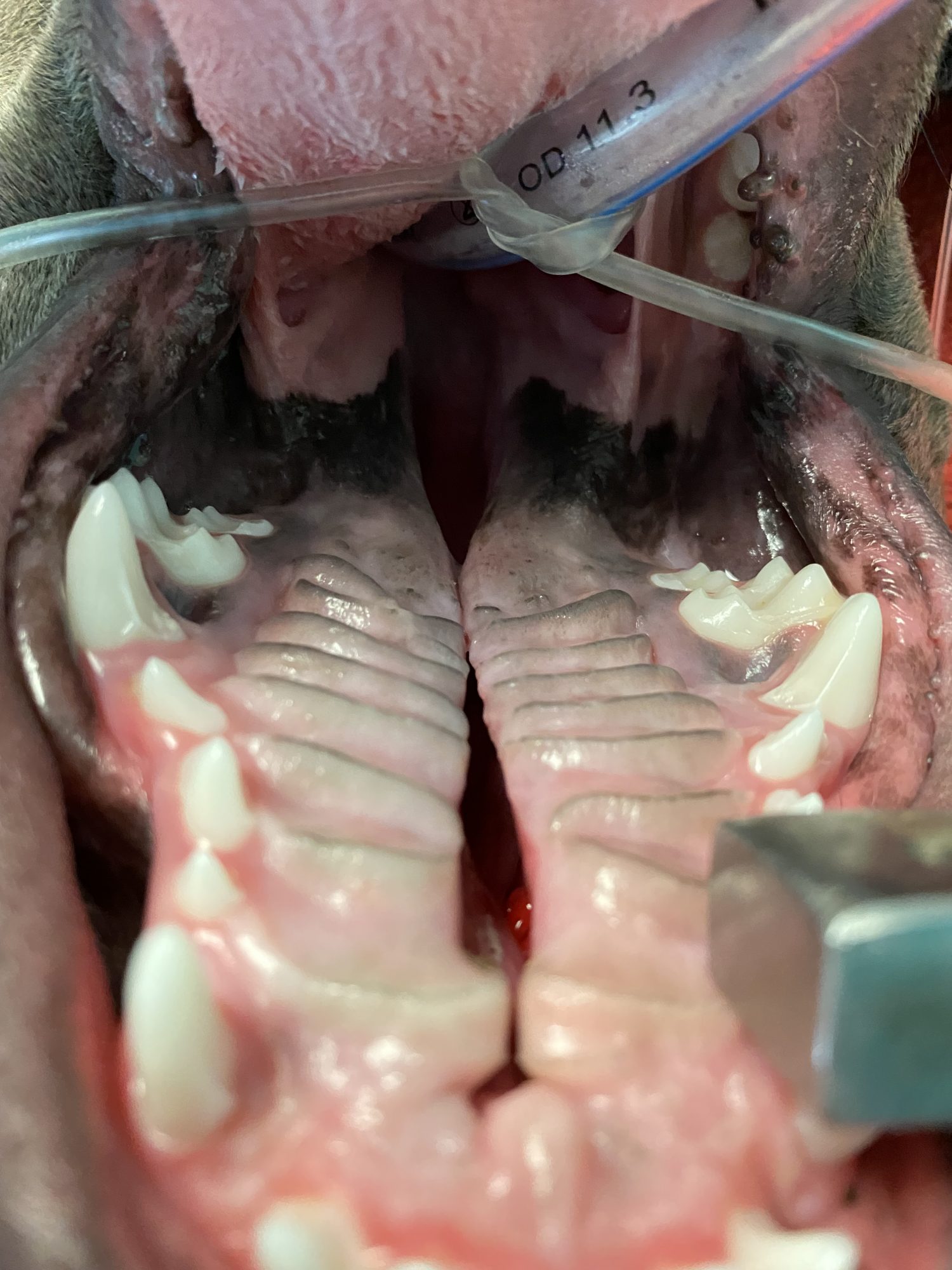
Puppies with a cleft palate cannot nurse properly, so they don’t grow as much as the rest of the litter. They are typically the “runt.”
Those who survive eventually can have discomfort, a reluctance to eat and drink, difficulty breathing, and ongoing infections. After all, the nose is not supposed to be full of milk or food…
His amazingly dedicated owner wrote: “Novakai was tube-fed until she was about 5 months old. At that time, small amounts of soft kibble were offered. Sadly, most of it would come back out of her nose. So she stayed on a pureed diet until she turned 7 months.”
The only good solution is surgery to reconstruct the hard and the soft palate.
The hard palate is the front portion of the roof of the mouth. It’s hard because there is bone behind it.
The soft palate is the back part of the roof of the mouth. It’s soft because there is no bone behind it.
Suturing one side of the defect to the other does not work. It is doomed to fail. The tissue is just too tight. So one solution is to rob (tissue) from Peter to give to Paul.
PICTURES BELOW ARE GRAPHIC AND ARE NOT FOR THE FAINT OF HEART.
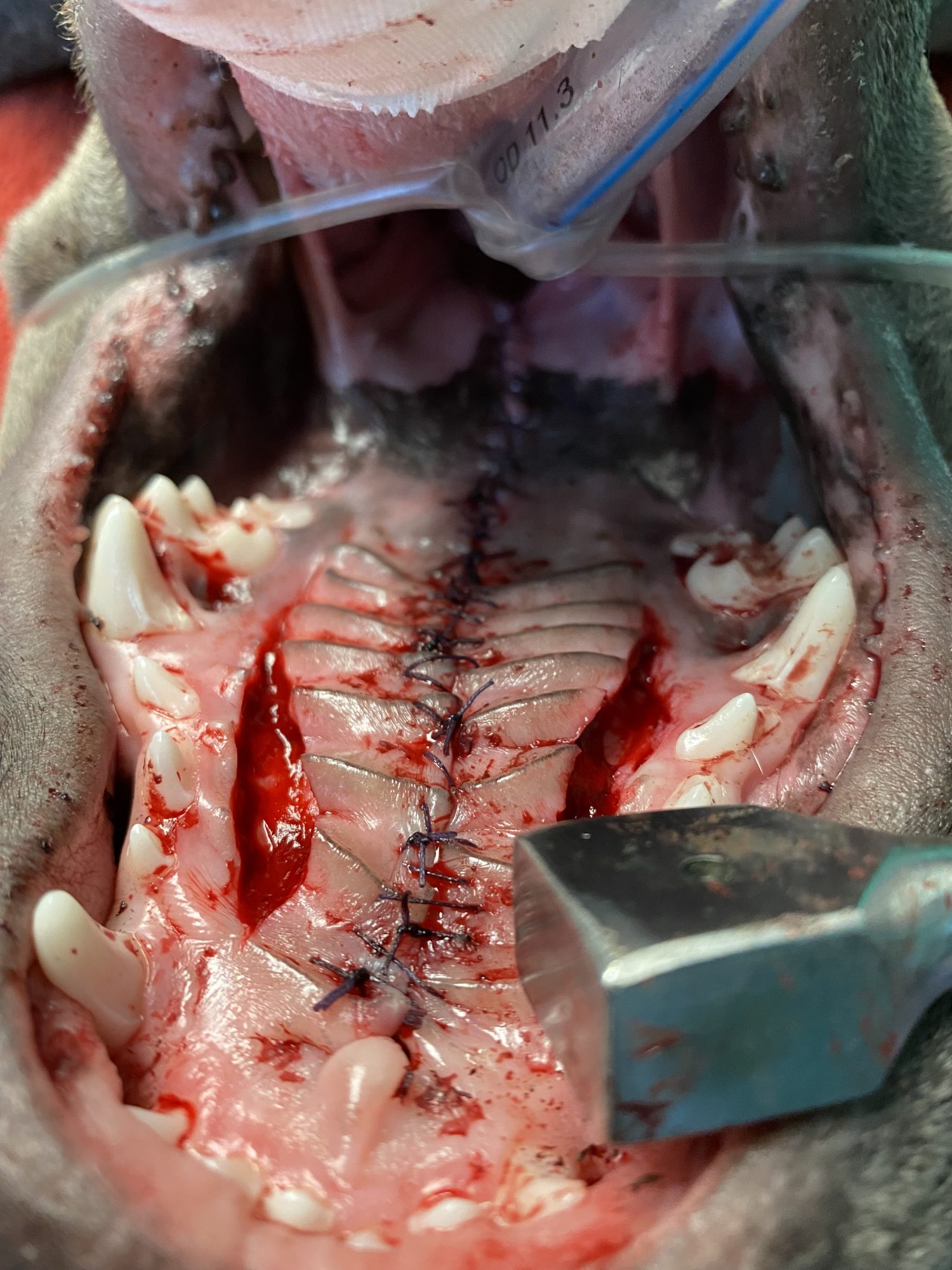
After creating incisions in the hard palate, we created 2 “flaps” or bands of tissue. Then it became easier to stitch one to the other, in the middle of the roof of the mouth.
This left an area on each side where the bone is literally exposed.
Amazingly, those healthy areas progressively heal with new tissue.
Novakai recovered smoothly after anesthesia and surgery, and went home.
She had to stay quiet for one month, without any chew toys or hard food to protect the stitches and the surgery area.
Thankfully, the mouth has an amazing ability to heal. Think of when you bite your tongue or the inside of your cheek. It hurts at first, but then it heals within days.
Novakai needed a bit longer than that, but the end result was rather impressive as you can see below.
One month after surgery, we examined her mouth under sedation to assess the surgery site.
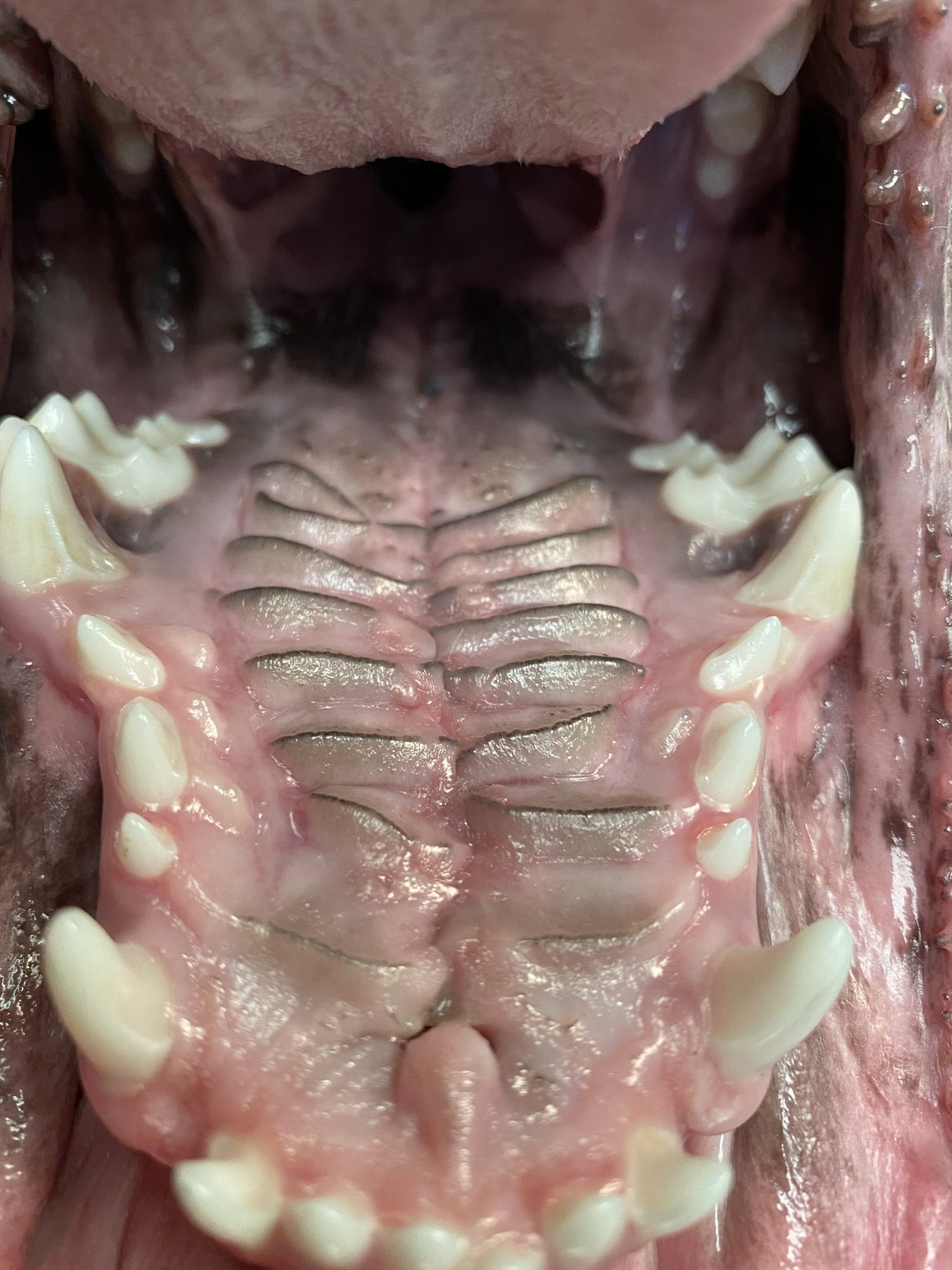
Thankfully, 100% of the surgery area had healed nicely.
Novakai’s owner concludes: “Today she is healthy, happy and very active. The surgery was a great success. She weighs in at a nice 60 lb. We are very pleased with the surgery. We knew the risk was 50-50. My family and I are all very happy that she turned out as well as she did.”
If you would like to learn how we can help your pet with safe surgery and anesthesia, please contact us through www.DrPhilZeltzman.com
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!

