Dr. Phil Zeltzman’s Blog
Pain is not acceptable
As a surgeon, my goal is to eliminate pain as much as humanly possible.
Let’s go over a few stubborn myths related to pain in pets.

1. My pet doesn’t cry out
“My pet is not crying and therefore is not in pain” has to be one of the most stubborn myths vets face on a daily basis.
When a pet limps or favors a leg or doesn’t put full weight on a leg, they are most likely in pain.
When a pet’s activity decreases, they may be in pain.
When a pet’s routine or habits change, they might be in in pain.
When a pet’s appetite decreases, they could be in in pain.
The fact is, most pets, especially cats, do not cry out when they’re in pain. Of course, if you step on their foot, they will cry out in pain, but that is short-lived because of what we call acute pain. Long-term, ongoing, continuous, sustained pain is called “chronic” pain.
Similarly, a dog may cry out in pain when (s)he initially tears a ligament, such as an ACL. But then the pain becomes subtle or low-grade and there’s typically no more crying.
Yet as long as they’re limping, it means that pets are in pain.
It’s the same idea as when you have a pebble in your shoe. You will shift weight to the other leg to decrease the pain. But as long as you put weight on the foot with the pebble, there will be some degree of pain.
Pain in cats is even harder to assess than in dogs. Cast tend to change their habits: less grooming, less jumping up or down, decreased appetite, hiding, fewer interaction with humans, withdrawal.
2. My pet is just old
Age seems to be the catchall excuse for multiple ailments. For example, urinating in the house is often blamed on old age, even though a bladder infection or bladder stones ( https://www.drphilzeltzman.com/blog/?p=1841) might be present.
When it comes to a pet’s decreased athletic ability – unwillingness to play, using stairs or jumping on furniture – many pet owners believe that age is the culprit.
Before we get to that conclusion, it’s important to make sure your pet doesn’t have a torn ACL, or severe hip dysplasia, or a bulging disc.

3. Pets don’t feel pain like we do
Some people still think that pets don’t feel pain like we do. Yet mammals have the same type of nerve endings, pain pathways and pain perception center in the brain as humans do.
To think that an animal in pain doesn’t deserve the same kind of treatment as humans is simply wrong.
4. There’s nothing we can do
Some pet lovers are told that because one pain medication doesn’t seem to work anymore, there are no other options.
Yet there are almost always other options: other pain meds, surgery, physical therapy, acupuncture, weight loss etc.
If all options have truly been explored, then maybe it’s time to have a discussion about quality of life, but not until then.
When the end finally does come around, you can rest assured that you truly did everything possible.
5. Postop pain is beneficial
Vets used to say that postop pain is a good thing because it keeps pets quiet, and that helps prevent injury to the surgery site.
We now have a much better understanding of the implications of untreated pain.
In my surgery practice, we routinely use 4-6 different techniques to prevent and treat pain. The drugs and techniques are well known, it’s just a matter of using them.
6. Minor procedures don’t need pain medication
This is another stubborn myth. Even what seems like a minor procedure, like a neuter, a mass removal or a tooth removal causes pain and should be treated.

7. Pain medication in old or sick patients is dangerous
There are multiple pain medications we can choose from. Each drug has potential side-effects, for example related to the kidneys and the liver.
This is a manageable risk. It’s a matter of pros and cons. We can easily monitor consequences on kidneys and liver with regular bloodwork. In a healthy pet on an anti-inflammatory, bloodwork is typically recommended every 6 months. In a pet with kidney or liver issues, bloodwork can be performed every 3 months, or even more often.
Another strategy is to decrease the dose of “risky” medications, usually an anti-inflammatory, or stop it altogether. We can also replace it with other, safer pain medications.
8. My client won’t pay for that
Some vets are concerned that you can’t afford proper pain prevention and treatment.
There, I said it.
If that is your case, then you should discuss it honestly with your vet.
If not, then you should demand the best possible pain management for your pet.
9. Surgery causes pain
A few of my clients have declined surgery for this reason.
As a surgeon, I’m not naïve enough to ignore the fact that left untreated, pain will occur after surgery. Again, most of my patients benefit from half a dozen pain management techniques.
This includes IV medications, special IV fluids, local pain meds, pain medications by mouth, pain medication injected directly into joints, pain medication injection around the incision etc.
So being fearful of surgery because of the fear of pain does not make sense. We can prevent and treat pain. In fact, a common reason to do surgery is specifically to treat pain.
Think of a broken leg. One consequence of surgery is to decrease the pet’s pain.
So it is quite the opposite: surgery helps decrease pain and eventually, it eliminates it.
10. My pet is not in pain
With all due respect, I would argue that many pet owners do not realize how much pain their pet is before surgery. Why is that? Possibly because everybody (humans and pets) slowly got used to it.
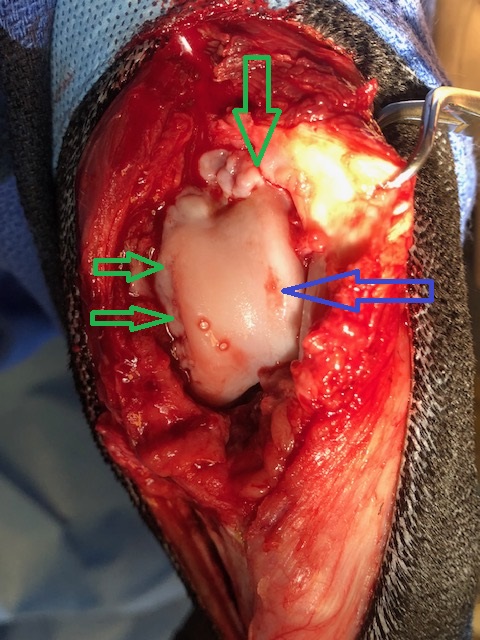
Case in point, we recently did a Total Ear Canal Ablation (TECA) in a Cocker with severe ear infections.
TECA is a pretty invasive surgery that has a reputation for being painful. So we use as many pain medications as possible, as mentioned above.
The very next day, the owner sent an email with an update: “He had a few rough moments trying to get comfortable. But once we got him to take his pain medication, he fell asleep and slept through the rest of the night.
(…) He woke up like a new dog today!
You would never even guess he had surgery. He had a full appetite, and is walking around very alert and actually attempting to play which we are trying to discourage at this point.”
Keep in mind, this comment came from a very smart, attentive and loving pet owner. She is very in tune with her dog. She was surprised by how comfortable her dog was after such an invasive surgery and went out of her way to email me to acknowledge how much pain her dog must have been in before surgery. And how comfortable he was after surgery.
This is actually one of vets’ biggest frustrations. We know when a pet is in pain and it’s sometimes difficult to convince a pet owner that their pet is in pain.
By the same token, if you feel that your family vet does not believe you that your pet is uncomfortable or painful, then it is your absolute right to seek a second opinion until you find somebody who takes you seriously (here is a perfect example: www.drphilzeltzman.com/blog/joshuas-story-taking-pain-seriously).
As I always say, “pain is not acceptable.”
We are extremely fortunate to have access to all kinds of pain medications and surgery options to make many pets more comfortable.
Here are 20 signs that your pet might be in pain
. Limping, favoring a leg
. Decreased social interaction, withdrawal
. Anxious facial expression
. Submissive behavior
. Decreased movement
. Decreased jumping (eg on the sofa, in the car)
. Difficulty doing stairs
. Decreased grooming
. Whimpering
. Howling
. Growling
. Guarding behavior (e.g. head shy)
. Aggressiveness, biting
. Decreased appetite
. Weight loss
. Self-mutilation (licking, chewing, biting an area)
. Changes in posture
. Dogs: constipation
. Cats: Changes in urinary/defecation habits
. Hiding
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
10 ways to help a pet with arthritis
About 30% of cats and dogs are affected with arthritis.

Before we discuss 10 ways to help, please remember: arthritis cannot be assumed. It has to be proven (X-rays are one good way).
Giving anti-inflammatory drugs to your pet just because somebody “thinks” (s)he is affected by arthritis is just not appropriate. There is no cure for arthritis, but it can be controlled. Here are 10 ways to help…
1. Weight loss or weight control
Extra pounds add pressure on joints with arthritis. Losing weight is then critical. Your family vet can help your pet lose weight (with weight-loss food), or maintain the weight (with a “light” diet). One classic research study showed that “in overweight dogs, weight loss alone may improve lameness.”
It is important to remember that the front legs support 60% of the weight, whereas back legs carry 40%. Therefore, weight loss is even more important with arthritis in joints of the front legs: shoulder, elbow or wrist (carpus).
2. “Arthritis” diet
Once your pet has an ideal weight, you can switch to an arthritis diet. These diets are typically enriched in glucosamine, antioxidants (such as vitamins C and E) and omega-3 fatty acids (fish oil).
Such diets are perfectly balanced, i.e. they have all the necessary nutrients, vitamins and minerals, so they can be fed for life. However, they are not appropriate for a growing pet, so they should be used in adults only.
Pro tip: there is now a special food that help with weight loss (or weight control) and arthritis at the same time – a major improvement.
3. Joint supplements
Because there is never enough glucosamine or fish oil in any pet food, it is important to give supplements by mouth in addition. We will recommend them after most orthopedic surgery to manage the arthritis.
Other supplements can be injected by your family vet.

4. Controlled exercise
Lack of activity leads to muscle loss, a decreased range of motion in the joints, aka stiff joints, and weight gain (if you don’t decrease the calories).
Despite the discomfort, it is very important to continue exercising. Generally, slow leash walks are ideal. You can progressively increase their duration. For example, start with 5 minutes 2-3 times daily for one week, then increase that by 5 minutes each week.
These walks help keep muscles strong and joints flexible.
Supervised swimming, or walking in wet sand, or tall grass, are another great ways of providing low impact exercise, as long as your dog doesn’t struggle to get into or out of the water. Encouraging exercise in a cat can be challenging, but some owners are able to train their cat to walk on a leash!

5. Physical therapy (PT)
Even though untreated arthritis causses pain, not moving is only going to make thigs worse.
Physical therapy is a great, gentle wait to move joints in a controlled way.
Done at home or at a physical therapy center, PT can make a dramatic difference. Most doggie physical therapists (officially called rehabilitation practitioners) will perform some exercises that can only be done at their facility, such as walking in an underwater treadmill, and will show you exercises to do at home. PT starts with a “warm up” and ends with a “cool down.”
If you have ever needed PT for yourself, you may appreciate how dramatic a difference it can make in your pet’s life. I have personally seen rehab practitioners perform small miracles on some patients!
6. Anti-inflammatory drugs
The most commonly used pain medications used for arthritis pain are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Ideally used on an as-needed basis, rather than every single day, modern NSAIDs are safer and more potent than aspirin & “people” drugs. By the way, please never use people drugs in your pet without your vet’s complete approval, especially in your cat. Some of these drugs can be deadly.
Potential side-effects of veterinary NSAIDs include vomiting and/or diarrhea, with or without blood, lack of appetite, lethargy or jaundice (a sign of liver disease), or kidney disease. Your family vet will typically perform regular lab work, testing blood and urine, e.g. every 6 months or more often in at-risk patients, to monitor possible side-effects.
7. Pain medications
When anti-inflammatory drugs cannot be used, or are not strong enough, other pain killers can be given (gabapentin, tramadol etc.). There are other options, which need to be tailored to each individual patient. Sometimes, it is a matter of “trial and error” until the ideal drug combination is found. Every patient is different, so there is no ideal solution that works on all patients.

8. Environment changes
Many small tricks can help. Keeping your pet in a dry and warm place should help, just like it would help an arthritic person. It is important to keep your pet on thick, soft, clean padding at all times, rather than on tile or linoleum (although some pets seem to prefer those!). Minimize access to stairs. Elevate the food & water bowls.
If you have a few steps on your deck, you could build a ramp. Some companies sell steps to help pets get onto furniture more easily. To get in the car or the truck, you can also use a ramp. Whether inside or outside, always provide good footing so your pet doesn’t “do the splits”. Hardwood floors can be covered with area rugs or yoga mats. And be extra careful on ice during the winter time. Pets can get seriously hurt after slipping on ice. An easy solution is to use a sling under your dog’s belly.
9. Periodic re-evaluations
Follow up exams with your vet are critical to adjust the plan to your pet’s progress. For example, if you are trying to make your pet lose weight, monthly weigh-ins are important to track your progress. The amount of food may need to be adjusted, otherwise the weight may just plateau if you continue feeding the same amount.
Similarly, pain medications could be changed or the dosage adjusted depending on your pet’s progress.
10. Surgery
In some cases, surgery is an excellent way to treat arthritis. From simple procedures (removing a flap of cartilage or part of a bone) to more complicated surgeries (fusing a joint, or a total hip replacement), ask your family vet or your surgeon if your pet would benefit from surgery.
So there you go: there are (at least) 10 ways to help a pet with arthritis. There are other modalities, such as acupuncture and stem cell therapy, which you can discuss with your family vet or your surgeon.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
How do I know if my pet is in pain?
This is a very common question… and it does not have an easy answer.
An entire book could be written about pain!

Instead of a book, here are some general, practical guidelines.
1. Limping
This is one of the most difficult message to convey. Yet it’s simple.
LIMPING = PAIN – 99% of the time.
2. Decreased activity
If your pet suddenly or progressively doesn’t play as much or as long as usual, it’s important to find out why.
3. Difficulty in stairs
To simplify, going downstairs puts more pressure on the front legs, so they may be the issue.
And going upstairs puts more pressure on the back legs, so they may be the source of the problem.
4. Changing habits
If your dog runs like a maniac to greet you when you come back from work every single time, and progressively or suddenly doesn’t, why is that?
If your cat loves napping on a window sill to enjoy the sun, every single day after breakfast, and doesn’t anymore, why is that?
If your dog loves going on a walk, or a run, or a bike ride, and doesn’t anymore, why is that?
5. Difficulty jumping
If your pet routinely jumps on the couch, or your bed, on in your car, or on a chair, and suddenly or progressively doesn’t as easily, it may be because of pain.
6. Difficulty getting up
Struggling to get up after a nap or in the morning, or stiffness in the legs, can also be a sign of pain or arthritis.
7. Change in appetite
Painful pets often lose their appetite, even for a favorite treat. It could be sign of pain in a leg (difficulty walking to you or to the bowl), or neck pain (reaching the bowl, which may need to be elevated), or pain in the mouth or in the teeth.
8. Not wanting to be touched
Pain can lead to “guarding” a leg or the belly, or becoming “head shy”. A classic example is a pet with ear pain or an ear infection (e.g. Cockers). Similarly, no longer wanting to be petted or picked up is a sign to take seriously.
9. Hunched position
A hunched position can be a sign of belly pain or back pain. Either way it can be very serious.
10. Reluctance to move a body part
This can apply to legs, and also to the neck. If your dog doesn’t like moving the neck up, down or to the side, and tend to look at you without moving the head, it can be a sign of neck pain.
11. Hiding
Cats are notorious for this. Either they hide, or they sleep in unusual places.
12. Grooming changes
Not grooming as much, or over-grooming or licking a particular body part can also be a sign of pain or arthritis.
13. Vocalizing
Crying or vocalizing may be a sign of pain, but PLEASE do not count on that to decide your pet is in pain. Many pets, if not most, will not cry when in pain.
14. Aging
Just kidding!
As I always say, “age is not a disease.” While slowing down can be normal, just like in people, limping or being in pain is not.
We can successfully treat countless conditions we were unable to help with before. You no longer have to accept your pet no longer playing or not wanting to go on walks because he or she is “just getting old.” It’s probably because they are painful or have arthritis. Both can and should be treated!
15. Off
Nobody knows your pet as well as you do! Sometimes, a subtle change, a gut feeling, a new routine, can give you an indication that something’s off.
Trust your instinct. Don’t brush it off. Ask yourself – or you vet – what this is happening. Everything happens for a reason in the pet world!
Here are a few more important points to keep in mind:
1. Hiding
Animals are very good at hiding when something is wrong. Remember, in the Wild, if an animal acts sick, they get eaten. Sadly, our pets have kept this ability. Cats are notorious for that.
2. Expression
Pain and its expression can vary dramatically from breed to breed, and from pet to pet. We know for a fact that some pets are more stoic, and others are more… “sensitive”.
3. Surgery
In my world as a surgeon, surgery is a classic way to help painful patients. Fixing a broken leg, repairing a torn ACL or removing a cancerous mass are just a few examples.
4. No surgery
But keep in mind that there are many ways to decrease or stop the pain without surgery including: weight loss, cold therapy, heat therapy, joint supplements, environmental changes, improving traction, acupuncture, harnesses, physical therapy, massage etc.
5. Warning
Please do NOT give any medication over the counter, or any human medication, or leftover medication from this or another pet, unless directed by your veterinarian.
Many human drugs are toxic to our pets, even deadly.
Something as “simple” as aspirin is a huge problem in a pet because:
1. We cannot give a better, safer, stronger anti-inflammatory drug for 7 days after stopping the aspirin and
2. If surgery is necessary, we cannot perform it safely for 7 days because aspirin thins the blood and increases the risk of bleeding!

ANY source of pain should be a reason to see your family vet or a board-certified surgeon.
As I always say, “pain is not acceptable.”
Pain should be taken very seriously – and vets are here to help you, help your pet.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Why is my dog crying after surgery?
“Doctor, I don’t know what to do, my dog keeps crying ever since coming home from surgery.”

This is a concern we occasionally hear after surgery. So why do dogs cry (or vocalize) after surgery? Note: we do not mention cats below, because, well, cats are different, so only part of what follows applies to cats.
1. Dysphoria
Dys what?
Dysphoria.
Dogs who wake up from surgery are discombobulated. They have no idea what happened to them. They’re spacey or groggy or loopy while the anesthesia medications wear off. They may not know who you are and where they are.
If you’ve ever had anesthesia, you likely felt the same way. You may also have seen videos of kids or adults waking up from anesthesia, after dentistry or surgery, and they say the weirdest or funniest things – which they don’t even remember later.
Since dogs don’t understand what’s happening, it causes anxiety. And they don’t know how to express that, except through whining.
While it’s stressful to any pet lover, the good news is that it should go away after a good night sleep.
If you doubt it, let me give you a classic example.
If we only sedate a dog (not even full anesthesia) to take X-rays or change a bandage or trim their nails, and reverse the drugs, they may experience dysphoria. We haven’t done anything painful, yet they cry like they’re in severe pain.
Why is that?
Well, it’s exactly for the reasons explained above. It’s dysphoria. They’ll get over it.
Bottom line: This type of crying should stop when you sit next to your dog, or you call his or her name.
2. Pain
Pain can definitely cause crying. Now, if your vet or your surgeon takes pain seriously, and provided appropriate pain control, the crying is most likely not due to pain.
As I always say, “pain is unacceptable in 2020.” We have enough pain medications available. We routinely dispense 2 or 3 pain medications to make sure your dog is comfortable after surgery.
If you are convinced that your dog is in pain, please call your vet and get an additional pain medication. That’s an easy solution.
Bottom line: This type of crying does not stop when you sit next to your dog, or you call his or her name.
3. Attention-seeking
Some dogs, like some babies (or older kids!) are quick at learning that if they whine, it makes you stop what you’re doing and you pay more attention to them. You pet them. You use your funny voice. You give them a treat.
It’s a learned behavior, which you encourage by “giving in.”
Bottom line: This type of crying should stop when you sit next to your dog, or you call his or her name.

There are other reasons for which your dog might cry after surgery. It can mean anything from “I hate this stupid cone around my head” to “I hate being locked up in a room/in a crate” or “Why do I have a 10 pound bandage on my leg?” or “I am bored to tears in here!” or “Why don’t you understand that I need to pee?”
So these are “benign” reasons that make them anxious. Again, they don’t know how to express their frustration besides crying. Other reasons include not feeling well, being unsteady, feeling nauseous, feeling cold.
Some breeds are more sensitive than others. And some individuals are more sensitive than others (“every patient is different”).
So depending on the situation:
. You may bring water or food closer. Some dogs need help when they wear a cone (which you should not take off). Handfeeding may help.
. You may want to give your dog a (safe) chew toy to prevent boredom.
. You can use white noise to drown out the normal sounds of the household.
. You can’t do anything about a bandage, although if it’s too tight, it can cause pain, so you should seek medical attention.
. You should absolutely follow your vet’s or your surgeon’s instruction to keep the cone on 24/7, or to keep your dog confined 24/7.
. If your dog needs to eliminate, then obviously you should allow that. Remember, you’ve trained your dog to be potty trained, so they may absolutely refuse to go on the floor or in their crate.
But be careful, as some smart dogs can learn that “whining = I can escape from jail and go outside” and they may take advantage of that.
Bottom line: This type of crying should stop when you sit next to your dog, or you call his or her name… or your take them outside to eliminate.
These are the main reasons for which a dog may cry. If you’re still not sure what’s going on with your dog, please call your vet clinic and brainstorm with a nurse to try to figure out why it’s happening.
The good news is that if you follow the rules, the whining should stop overnight or within a few days. If it doesn’t, then I’ll give you 2 more options:
. The reason for the crying is not listed above, and you need to figure out what the cause is by talking to your veterinary team.
. All we need is a mild sedative or tranquilizer to “take the edge off” and help your dog relax and accept their new fate: the plastic cone, confinement, a bandage etc.
After all, waking up from anesthesia is not fun for humans, so there is no reason to believe that it’s any more fun for a patient who has no idea what just happened.
Again: this is normal and it will get better with time, so hang in there!
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!

