Dr. Phil Zeltzman’s Blog
Will Weez need an amputation?
Weez, a cute 12 year old Cockapoo, had a swelling under her left armpit (aka the axilla).

No signs were present otherwise: she was eating, drinking and acting normally.
Since the swelling continued to grow, her owner wisely went to see his family vet. She diagnosed a mass of unknown origin.

The vet (again, wisely), recommended surgery to remove it and biopsy it.
The suspicion, based on experience, the location of the mass and its fast growth, suggested that it was likely a cancerous mass (soft tissue sarcoma, nerve sheath tumor, lymphoma etc.). In addition, there was a chance that it involved some important nerves in the armpit (aka the brachial plexus).
Since those nerves cannot be sacrificed, we discussed a small possibility of amputation.
A physical exam and blood work confirmed than Weez was a good candidate for anesthesia.
To my relief, my own exam revealed that there was no need to sacrifice the leg!
So we removed the mass uneventfully, and it as sent to the lab for analysis.

Weez recovered smoothly from anesthesia and surgery, and went home.
Her activity had to be restricted and she had to wear a cone (E-collar) around her beck for 3 weeks. She was also given oral antibiotics and pain medications.
One week later, the results of the biopsy were shocking – in a fantastic way!
Amazingly, the mass was benign! It is called a fibroma, which is a non-cancerous tumor, and very unusual in that location.
There is still a small risk that the tumor can come back, so I asked Weez’s owner to monitor the area by feeling it monthly.
Weez’s owner was ecstatic. He wrote: “Cannot be any happier and blessed to have had Dr. Zeltzman operate on our girl. He was able to remove a tumor and save her leg from being amputated.”
This story reminds me that board-certified cancer specialists (oncologists) and surgeons have 2 similar sayings:
* The 3 deadliest words in the English language are “Just watch it” and
* The 5 deadliest words in the English language are “Keep an eye on it.”
What we mean by that is size doesn’t matter when it comes to masses.
A tiny mass the size of a grain of rice can be cancer.
Bottom line: even though this mass was luckily benign, it is important to remove masses as soon as possible. Have your family vet check your cat or your dog as soon as you notice any lump or bump, so that they can guide you through the next steps.
So please don’t procrastinate. Removing a mass when it’s small is less invasive, less costly, and gives much better chances for a cure.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Khloe’s story: shocking findings nobody expected
Khloe was a 2 month old adorable golden retriever puppy, with a soft look in her eyes.

When her owners purchased her, they thought they were bringing home a happy and healthy puppy.
But as soon as Khloe’s family brought her home, they noticed that something was not right. She was not playful. She was quiet and reserved.
What they saw was a terrified, sick, and painful puppy.
An owner’s touch is supposed to comfort a small puppy. But how can that be when the smallest contact causes severe pain?
In a matter of 3 days, Khloe began having fits of screaming and jaw chattering. The smallest touch anywhere on her body caused her terrible pain. Her front legs were weak.
Khloe’s case was perplexing. Figuring out where the pain was coming from was almost impossible. It seemed that her whole body was affected.
The owner had noticed a small scratch on the skin of the head, sustained after a brief fight between Khloe and their other dog. It didn’t look like much and was already healing.
To help with the pain, I placed her on pain medications, and created a neck brace for her. It was difficult to tell, but it seemed that her pain might be stemming from her neck or her head.
Once Khloe was stable, she was transported to get an MRI of her head and neck.
When the MRI report arrived, we were shocked.
Khloe had several skull fractures, with severe changes in her brain, including encephalitis (irritation of the brain) and too much fluid. It was suspected to be due to an infection, most likely caused by the dog bite.
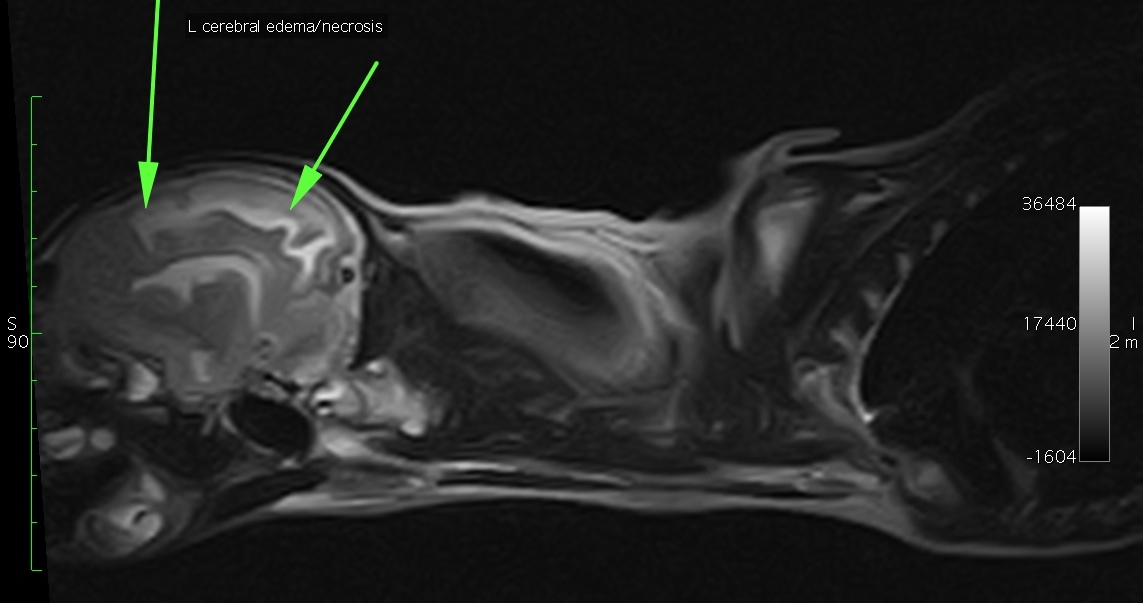
In addition, a brain abscess was suspected.
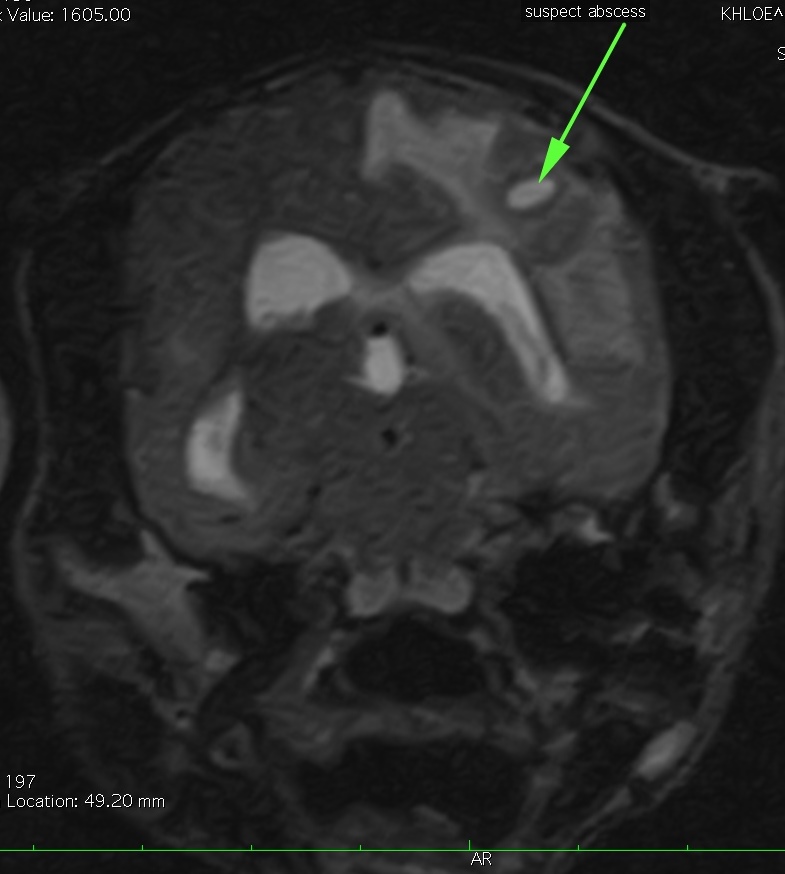
Suspected abscess
She had a mild displacement (hernia) of the back of her brain, called the cerebellum. And she had a severe syringomyelia extending caudally to the 8th thoracic vertebra (ie the middle of the chest).
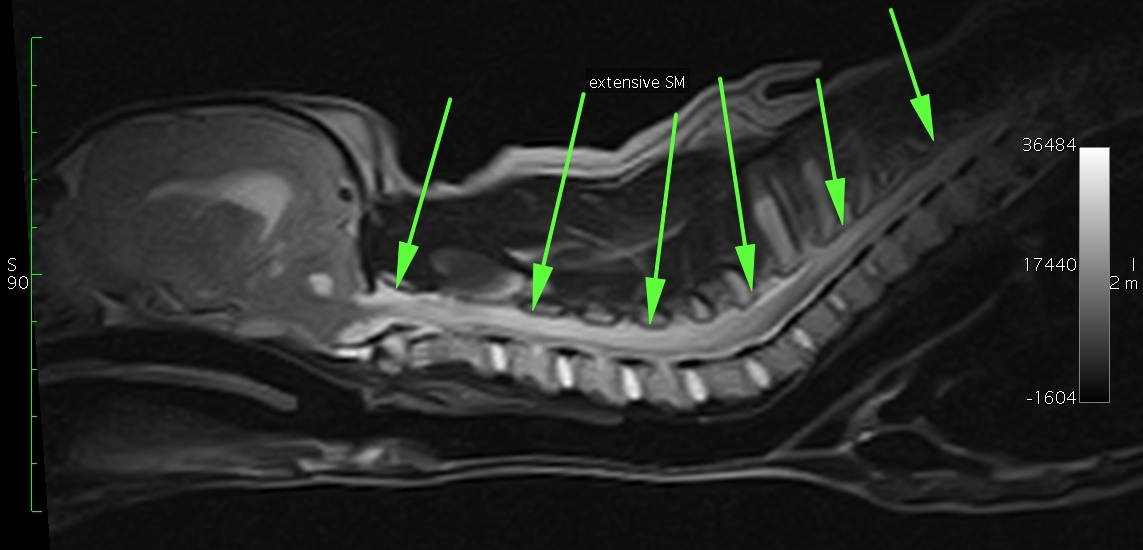
Syringomyelia is a condition that is due to fluid-filled cavities in the spinal cord, usually in the neck. This disease is most often found in Cavalier King Charles Spaniels.
So what we suspected was that a brief fight was in fact violent enough that it caused skulls fractures, and in turn a serious infection of the brain.
Based on these findings, Khloe was immediately started on medications. Two antibiotics were chosen to treat the infection. Two pain killers were also prescribed. One of them is called gabapentin, which is often used to control syringomyelia.
Three weeks later, Khloe was doing great and was finally behaving like a 3 month old puppy should!
It is difficult to tell at this point whether the syringomyelia will be a life-long issue or not. For now, Khloe’s owners are taking it one day at a time. They are thrilled that their pup has beaten the odds.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Sparky receives the gift of life
It’s lar par season!!!
As the weather gets warmer, I will see more and more dogs suffering from laryngeal paralysis.

This reminds me of a recent patient with lar par, Sparky, an 11 year old Labrador. He was suffocating and was diagnosed with laryngeal paralysis. This is a serious and stressful condition where the larynx (voice box) doesn’t allow enough oxygen to flow into the lungs.
His condition had been getting worse for about a year, then it suddenly got dramatically worse. When he arrived at Barton Heights Veterinary Hospital (www.bartonheights.com) in Stroudsburg, PA, Sparky had to be placed on oxygen. He was given tranquilizers to decrease the stress of suffocating.
Then something unusual happened. Because he was still struggling, he had to be placed under general anesthesia so that more oxygen could be delivered through a tube placed down the throat and into the windpipe.
This bought time until I was able to drive to the hospital and perform emergency surgery. The goal of surgery is to open up the larynx with permanent sutures (tie back surgery).
Despite a stressful start, Sparky’s surgery and recovery were uneventful.
And that was exactly 2 years ago,
His owner updated us after a year: “Sparky is still with us. We celebrated his one year anniversary last night with some vanilla ice cream. He has lost a lot of his muscle in his back end, but is still ambulatory and it hasn’t stopped him from trying to chase deer in the meadow (though he doesn’t get too far) or climbing up on the furniture (even though he has a comfy bed on the floor).”
How does his owner feel about doing the surgery on a senior dog (11 years of age), in spite of how severe his situation was a year ago?
“It really is miraculous! We are extremely happy – beyond words, really – that Sparky had the surgery and survived the ordeal. If he had lived only a week, or a month after surgery, we would not have regretted his having it, but the fact that he is here a year later certainly underscores why he should have had it. We are so grateful to you for the gift of his life!”
You can watch a quick video of Sparky here: https://youtu.be/fy7dWlAVqnM
So Sparky is breathing well. Yet “He has lost a lot of his muscle in his back end.”
It is possible that he has another nerve condition, related to lar par, that leads to progressive weakness in the back end (visit https://www.cvm.msu.edu/scs/research-initiatives/golpp/living-with-golpp for more info).
Sadly, there is no treatment. Well, besides doing the opposite of what most dogs wants to do: these dogs should not be moping around all day. They should be taken on slow, steady leash walks to keep the muscles as strong as possible.
Few pet owners are as dedicated as Sparky’s owner. She wasn’t about to give up on him without a fight, and the reward is a happy, breathing, deer-chasing Labrador!
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Cartier and the giant surprise…
Cartier, a 12 year old, 10 pound Shih Tzu, was originally seen by her family vet for a walnut-sized mass on the right side of her chest. It looked like a simple skin mass.

But she soon developed some rather troubling symptoms that had her owners seriously worried. She became lethargic, had difficulty breathing, and even passed out on occasion. What was happening?
Cartier was taken back to her family vet, where X-rays and blood were taken to find out what was going on. The blood work was normal, but shockingly, X-rays revealed that Cartier’s skin mass extended deep into her chest. It was so large, that it crossed to the other side of the chest!
The X-ray below shows the skin mass (green arrow), the chest mass (red arrow) and the heart (blue arrow).
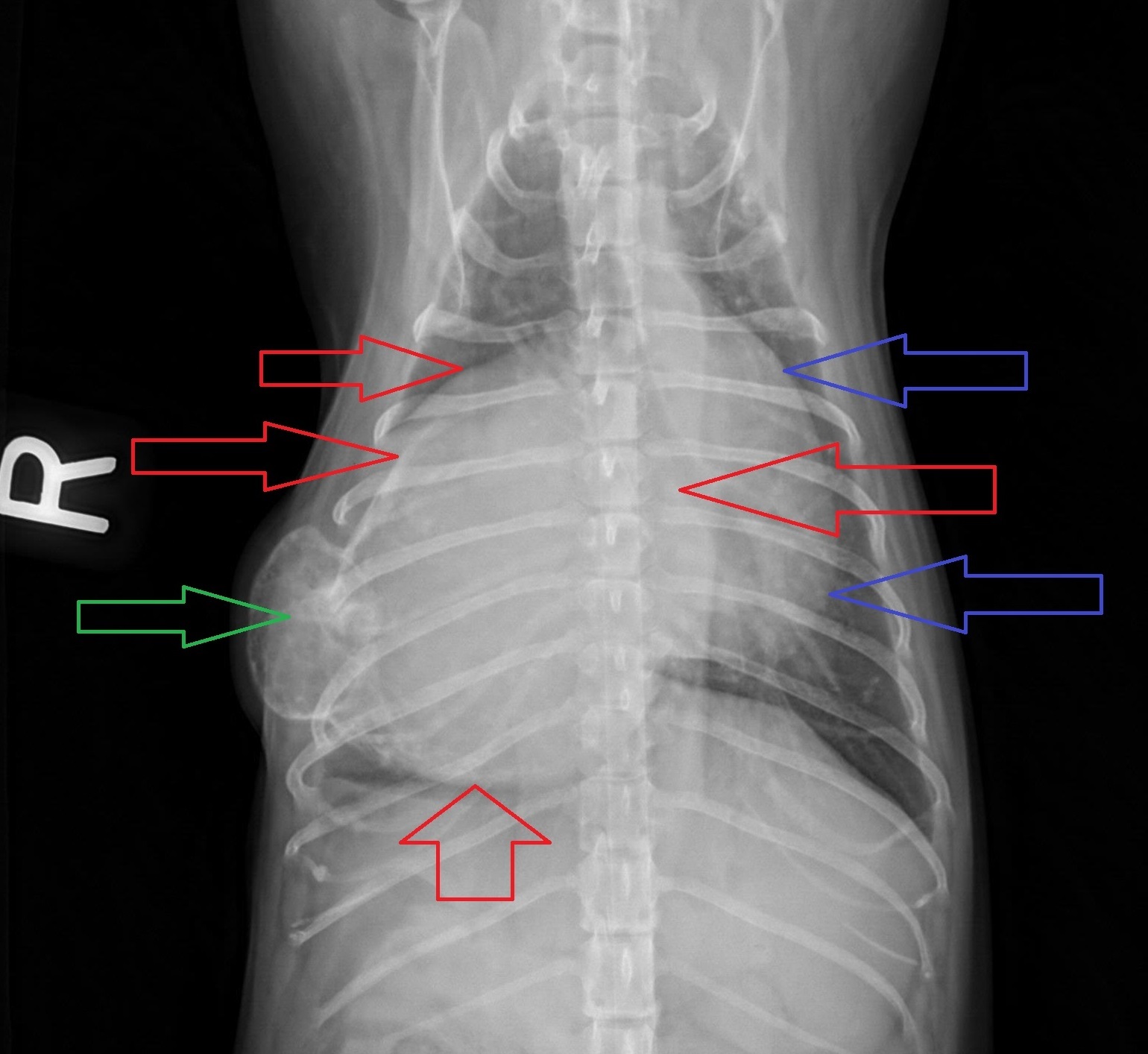
A cat scan of the chest was then performed to better understand what was going on inside the chest, and to make sure the mass had not spread anywhere. There was only one mass (between the colored arrows) but it was almost three times the size of her heart! This explained her symptoms. The only option to help Cartier was to remove the mass.
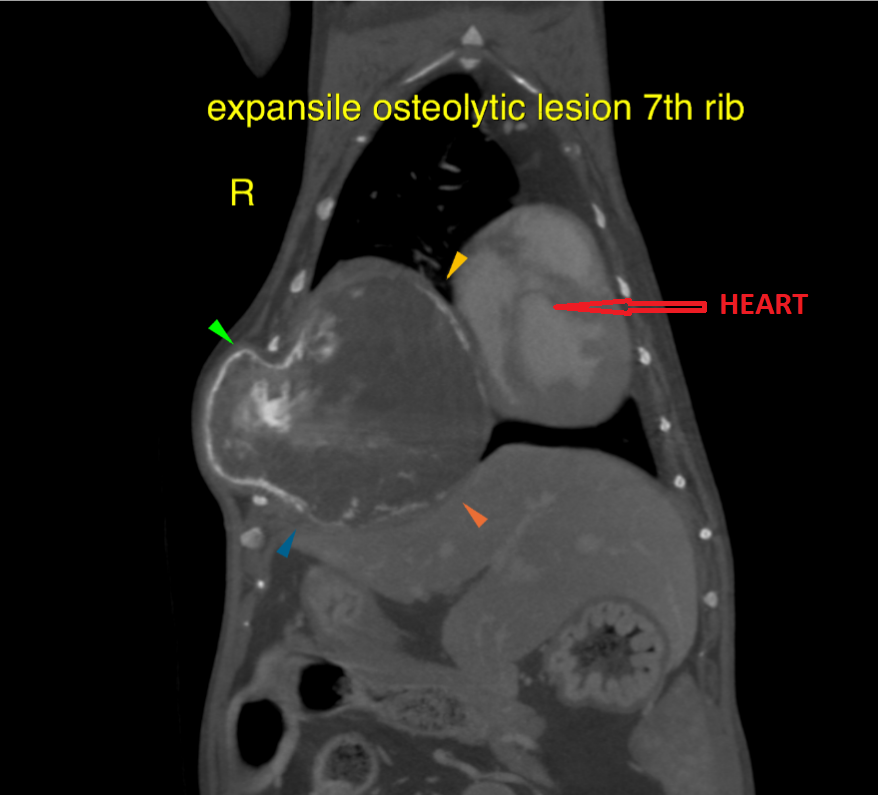
So I was called in to perform the surgery. On X-rays and on the cat scan, the mass appeared to involve a single rib, but that meant that several ribs would have to be removed in order to successfully remove the mass.
A total of 3 ribs had to be removed, along with the mass, without damaging the heart, the lungs, or any other vital structure. And remember, Cartier only weighed 10 lbs…
By the time we got done, the defect in the chest wall was so big, that it was not possible to put the remaining ribs back together. So the defect was reconstructed with nylon mesh in order to close the chest cavity.
Next, air from her chest had to be removed to allow her to breathe on her own once anesthesia was over. So we used a special plastic drain called a chest tube. Surgery was delicate, but it went well and Cartier bounced back remarkably quickly for an older lady. This is a video of her, walking around the day after surgery (chest tube still in place).
The chest tube was removed a few days after surgery and she went home safely.
The mass was sent to the lab to be biopsied. One week later, the results came back as bone cancer (osteosarcoma). This was one of the 2 most likely diagnoses. The other most likely possibility was cartilage cancer (chondrosarcoma).
One month after surgery, Cartier’s owners were happy to report that she had more energy, ran around, had bright eyes, and seemed to be back to normal. Her personality had come back, she had a hop in her step, seemed much more comfortable and no longer struggled to breathe.
Twelve year old Cartier now had a new lease on life.
Her owners said: “we couldn’t have asked for better results.”
Addendum:
I am thrilled to report that as of July 2019, Cartier, the now 13 year old, is still doing well.
This is 7 months after surgery.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
What you need to know about “bloat”
A surprising number of pet lovers have dogs at risk for “bloat”, yet they don’t know much about the condition.

If you own a dog at risk, it is very important for you to know about it.
What is GDV?
Bloat is a life-threatening condition with many synonyms, including twisted stomach, gastric dilatation and gastric torsion. The medical expression is Gastric Dilatation Volvulus (GDV), which is what vets typically call it.
In this condition, a dog’s stomach distends with air to dramatic proportions (see X-ray). This is called gastric dilatation (GD). An X-ray of the belly would show a “single bubble”, which means that the stomach contains air in a single “pocket”.
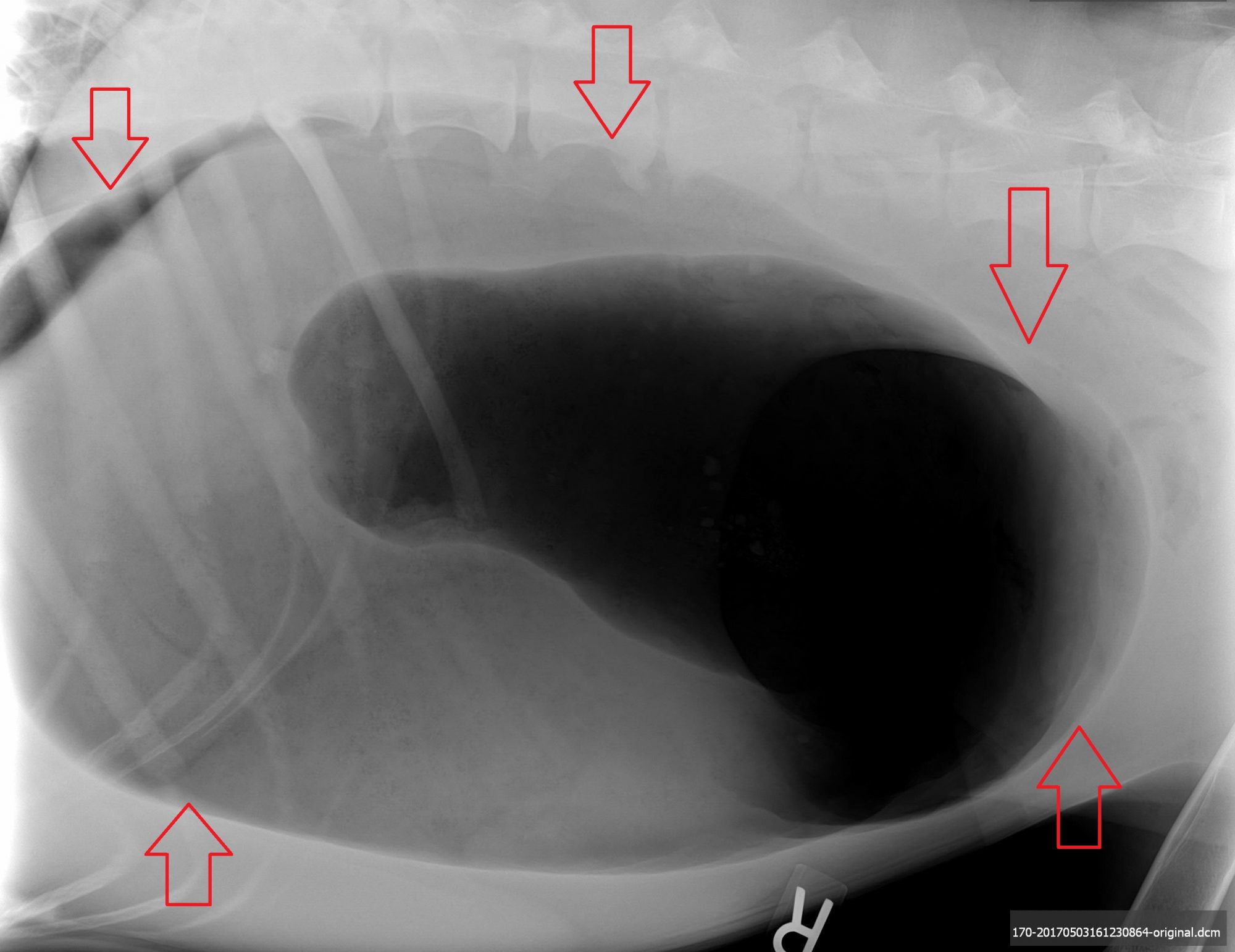
A classic example of the “single bubble” of GD in a German Shepherd. The arrows show the size of the stomach
The stomach can also twist onto itself, cutting off blood supply to the stomach and other major organs. It also blocks the exit of air and stomach contents. This is called Gastric Dilatation Volvulus (GDV). An X-ray of the belly would show a “double bubble”, which means that the stomach contains air in 2 separate “pockets”.
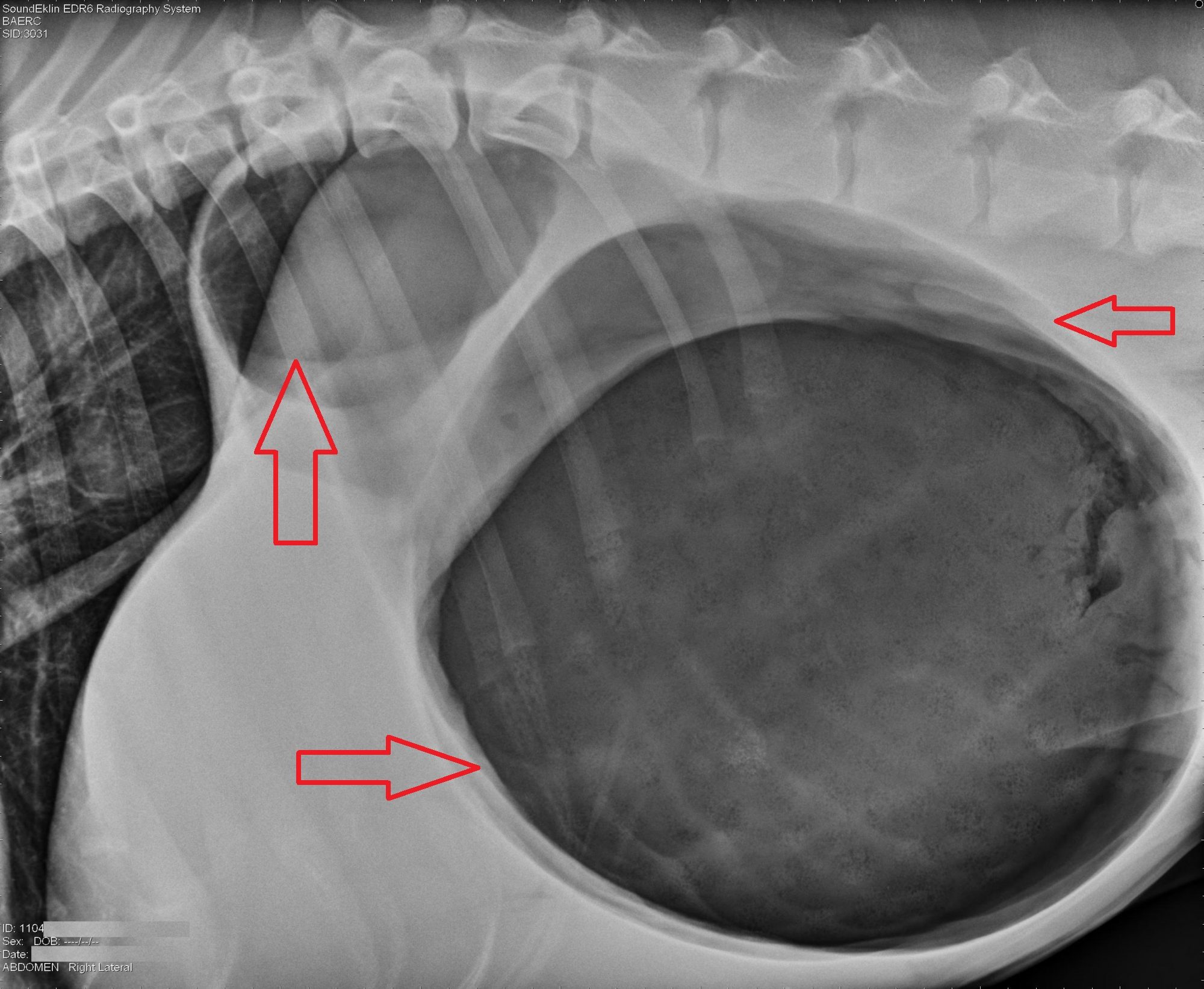
A classic example of the “double bubble” of GDV
Obvious signs of GDV include a huge (bloated) belly and “retching”, which means unsuccessful attempts at vomiting.
Less obvious signs of GDV include pacing, salivating, restlessness, inability to lie down, a distressed attitude, rapid breathing, and pale gums.
What causes GDV?
There are many risk factors. Some are questionable if not plain ridiculous. Here are a few scientifically proven causes of GDV.
* Large and giant breeds are at higher risk for developing GDV. Breeds such as Great Danes (the number 1 breed), Mastiffs, German Shepherds, Old English Sheepdogs, Weimaraners, and St. Bernards are all at risk but it also occurs in smaller breeds like Boxers, Basset Hounds and Standard Poodles.
* The disease is related to the dog’s body conformation, i.e. his or her shape. Deep chested dogs are more likely to have GDV. This picture of a Great Dane is a great example of what we mean by deep chest.

* Developing GDV can also be partially genetic: a dog related to a dog who suffered from GDV is at a 20% higher risk.
* Stressful situations or environments can contribute to GDV. We know that dogs who are boarded can bloat, possibly from being stressed out. The same applies to storm and fireworks.
* Food and water intake have been a commonly heard cause of GDV. Rapid eating, once daily feeding, and the type of food given can all be a factor in GDV risk. Too much water prior to vigorous exercise or prior to/during meals are believed to play a role in the development of GDV.
* Age can play a role in GDV. As dogs age, they experience some changes in their abdominal cavity (e.g. stretching of ligaments of the stomach), which can increase their risk.
Prevention
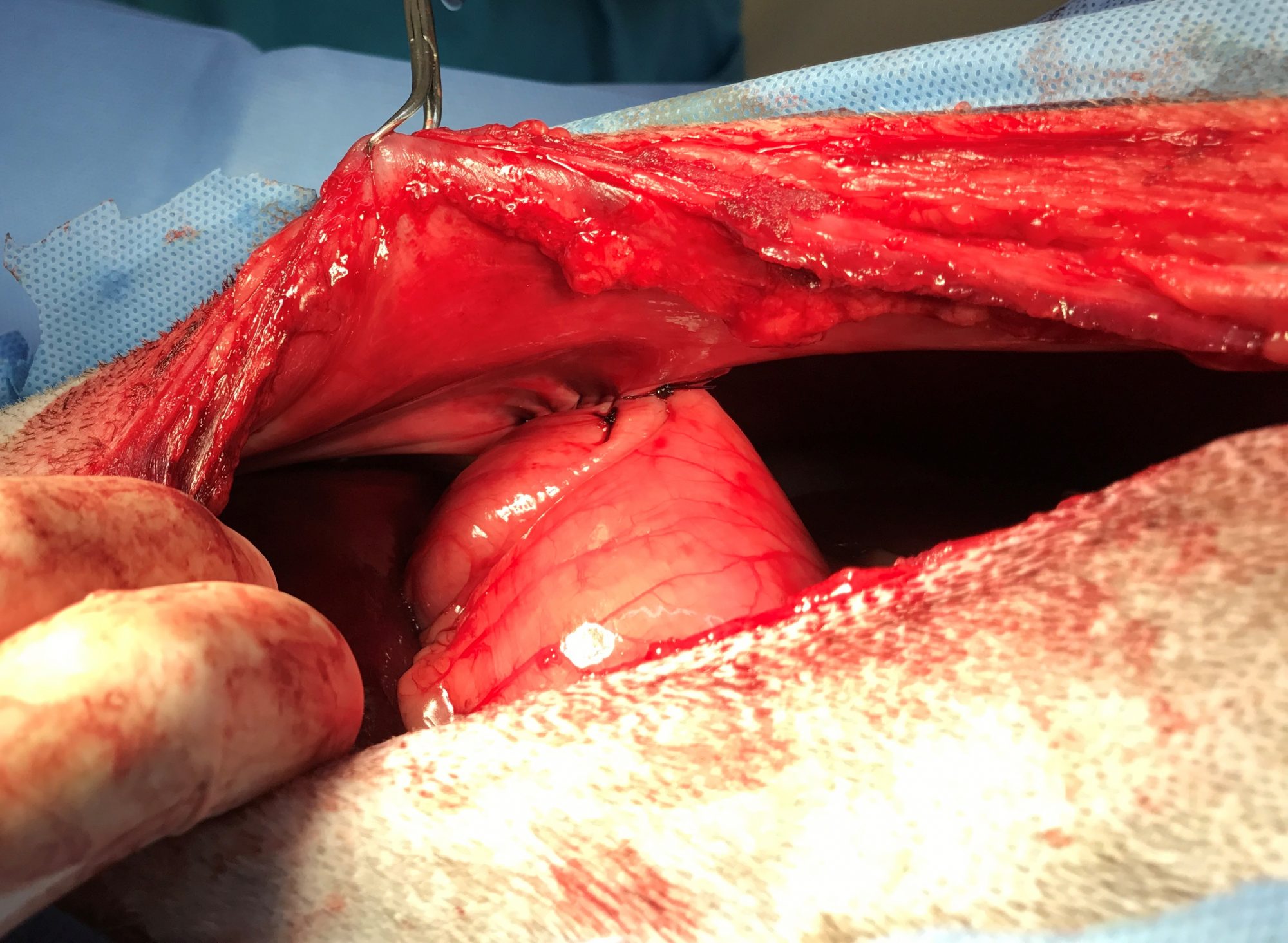
While scary and life-threatening, the twisting of the stomach can be prevented with surgery. Dogs at a higher risk for suffering from GDV can have a preventive surgery called a prophylactic gastropexy, or “pexy” for short.
This surgery entails stitching the stomach to the inside of the belly. When performed by someone experienced, it dramatically decreases the risk of the stomach twisting. This simple procedure can be done at the same time as a spay or a neuter.
The picture below shows the end result of a prophylactic gastropexy after a recent patient of mine, Zeke, a 1 year old German Shepherd, was neutered.
Very importantly, the dog can still “bloat” (a terrible, very misleading name) after a prophylactic gastropexy. It’s meant to prevent the twisting, not the “bloating.”
Should it happen, the dog must be rushed to the closest vet or ER to pass a tube into the stomach to remove the air, followed by stabilization with IV fluids etc.
Treatment
If a dog’s stomach has distended and twisted, surgery entails:
. Removing the air from the stomach ASAP.
. Repositioning the twisted stomach in its natural position.
. Performing a gastropexy (see above).
. Assessing the spleen, which can be damaged and may need to be removed.
. Looking at every organ in the belly to make sure nothing else needs to be addressed (“exploratory laparotomy”).
For additional information about Gastric Dilatation-Volvulus, follow this link to read a more in-depth article I wrote for veterinarians:
www.veterinarypracticenews.com/what-causes-gastric-dilatation-volvulus
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!

