Dr. Phil Zeltzman’s Blog
When is it time to say goodbye?
Nobody likes to talk about it. Once we realize that our pets are, after all, not immortal, we may hope that they will just “go” in their sleep. Well, that almost never happens. Most of the time, we have to help them. Euthanasia is a very personal, heart-breaking, grueling decision. Let’s go over 16 common concerns and questions.

1. What is euthanasia?
According to the American Heritage Science Dictionary, euthanasia is “the act of painlessly ending the life of an animal who has a terminal illness or incurable condition, as by giving a lethal drug”.
I would say that euthanasia, or “putting a pet to sleep”, is the humane way to end a pet’s life with dignity when their quality of life is no longer acceptable. Euthanasia should not be a convenience when a pet becomes, well, an inconvenience.
2. When is euthanasia appropriate?
It’s all about quality-of-life. A quality-of-life scale helps you assess various criteria such as pain level, appetite, hygiene, happiness, mobility etc.
You can Google “quality of life scale HHHHHMM” to find a great example.
Basically, are there more good days or bad days? The challenge is that you need to try to look at the situation from your pet’s standpoint – not yours.
This is often difficult, because it is a very emotional situation that tends to make you lose your objectivity. In other words, if the same situation happened to your best friend’s pet, you probably would know exactly what to do. But because you are dealing with your own pet and your own emotions, you cannot see the situation as objectively. Sometimes, denial makes things even worse…
3. When will I know it’s time?
Some people say “You’ll know in your heart when it’s time.”
I’m not so sure it that’s easy. Sometimes, you just don’t know. Again, you are so emotionally close to the situation, that you often can’t reason with a clear mind. Therefore, some pet lovers just don’t know when it’s time.
It is a vet’s job and ethical responsibility to make the owner aware of the situation. It is however not a vet’s job to make the decision for a pet’s owner. So asking “What would you do if it were your pet” is usually not a fair question: it’s a very personal decision.
The vet’s job is to explain the facts, describe the medical situation, and present options. Only you can (and should) make the final decision.

4. How is euthanasia performed?
Each vet has his or her own protocol, so the description below is only one way to do things. Let’s try to forget emotions for a minute, and let’s try to focus on the scientific or medical aspect of euthanasia, so that you know what to expect.
An IV catheter is placed. Most veterinarians will give a sedative or tranquilizer IV first, to relax the patient, or even make them sleepy. Then, the euthanasia drug – an overdose of barbiturates – is given IV. This is a pain free, almost instant procedure. The heart and lungs stop. And it’s over. I think most pet owners are surprised how quickly euthanasia happens. It’s over in less than a second…
You may then want to spend some time alone with your pet to say goodbye.
Although not exactly glamorous, it is important to mention a few things that may or may not happen during euthanasia. For example, your pet may or may not have one last deep breath (called an agonal breath). Eyes typically don’t close. This is not Hollywood.
There may be noises or vocalizations, or muscle spasms, or urination, or defecation, as the body relaxes. These are just possible, physiological, medical things that can happen and may be traumatizing if you are not prepared or warned.
Regardless, euthanasia is a quick, smooth & painless process.
5. What do I do at the animal hospital?
An experienced team will guide you through the different steps. Here are two important suggestions:
. Ask if you can take care of all the paperwork and financial stuff BEFORE proceeding with the euthanasia. The last thing you want to do is stand at the front desk after the euthanasia, in tears, in the middle of a full waiting room. A good receptionist should spontaneously suggest this option.
. Have a friend or family member drive for you if you think you will have difficulty driving safely after it’s all over. Now is not the time to get teary-eyed and get into an accident!
6. Should I be present?
This is one of the most difficult questions to answer. There is no right or wrong answer. There are several options.
You can say goodbye, leave the room, and let the doctor proceed. You may or may not want to visit afterwards. Or you can be present, start to finish.
Here is a testimonial from a friend and former client in Cincinnati, OH:
“My daughter and son-in-law had to euthanize Banshee, their Bernese mountain dog. They had had his leg amputated, but the cancer progressed. In the end, they had to put him to sleep. It is always sad to lose a pet. He was one of the sweetest dogs I’ve ever known, and even in his illness, he kept his sweet disposition.
My son-in-law and daughter were both with him at the end. That is something I would encourage pet owners to do. It is a comfort to see how peacefully your pet can go, and for me their loyalty demands your presence. I recognize that some people may not be able to do it.”
7. A very special situation
In our surgical practice, there is another situation. We are occasionally faced with an incurable condition during a surgery. I will then call the owner on the phone during the surgery, discuss the situation, and if we both agree, humanely euthanize the patient “on the table.” In this situation, the patient goes from anesthesia to euthanasia with no awareness and no pain whatsoever.
Here is a testimonial from a client who had to make such a decision. Their cat Jackie needed surgery to remove a fibrosarcoma – a cancerous tumor – from the skin of her belly. It turned out that the tumor invaded multiple structures, including half of her diaphragm (the muscle that separates the chest and the belly). The cancer was inoperable.
The owner writes: “I was faced with a very difficult decision.
My kitty Jackie was on the operating table when I received a call from Dr. Zeltzman, telling me that the tumor she had was so extensive that he did not feel he could remove it all. Compassionately, he gave me my options:
#1 – He could wake her up from surgery and let her live out what would be the rest of her life. The tumor however would eventually cause her significant pain.
#2 – Put her to sleep now while she was still under anesthesia. He told me I could think about it for a bit and call him back with my decision.
I tried my husband at work, but was unable to reach him. I kept thinking about Jackie and that she was so young, only 7 years old. I thought about how she came to be my kitty. (…) She was my side-kick.
With Jackie still on the table, I called Dr. Zeltzman back. He talked me through my options, not making the decision for me, but helping me make the right decision. After my conversation with him, I decided to have Jackie put to sleep then, while still under anesthesia. My deciding thought: I did not want Jackie to suffer.
It has been two months since that day. I miss her so very much! The hardest part for me was that I did not get to say goodbye to her. But in my heart, I know I made the painful but right decision for Jackie. I take great comfort in that.”

8. What happens with the remains?
There are several options. Some people elect to bury their pet. This may be illegal where you live, so it is important to check. It you can’t, there are memorial gardens and cemeteries for pets throughout the country.
Most owners elect cremation. You then have 2 options: you may get ashes back, or not. Some people save the ashes.
Here is what a pet owner wrote after receiving her pet’s ashes. Cookie, a 1 year old female Boston terrier, had abdominal surgery that revealed a terrible condition called intestinal volvulus: 90% of her small intestine had twisted onto itself, which is deadly.
The owners were called during the surgery, and reluctantly elected the only reasonable choice: euthanasia. Later, they write:
“Cookie’s ashes now sit on our mantle in the beautiful box with her name on it. (…) Cookie has come home in style.”
Other pet owners sprinkle the ashes somewhere, such as the pet’s favorite place in the back yard. Again, this is a very personal decision.
9. What happens during the grieving process?
For most clients, losing a pet is like losing a family member, so the grieving process should not be taken lightly.
Typically, people who do not own pets don’t understand how sad a grieving pet owner may feel. This may be a good time to avoid such people, for example at work…
10. Where can you get support?
Support is crucial to get over a pet’s loss. It can require finding a friendly ear: a friend, a family member, a receptionist or a nurse you developed a good relationship with, or your family vet.
If you have other pets, they can also provide a support system, as you will need to redirect your attention to their needs. Actually, your other pet(s) will “feel” that their buddy is missing, and they will feel your sorrow. Now is the time to provide some extra TLC. They may become lethargic or have a poor appetite.
Your other pets may actually help you grieve, so you can actually help each other.
There are also some websites where you can share your feelings.
If you are completely overwhelmed, or you feel that you are grieving for an unusually long time, you may need counseling. This is now available through several vet schools and of course through a private counselor.

11. What can I do to get through this?
Here are a few things you can do to help you heal.
. Allow yourself to cry. It’s okay – really.
. Put your pet’s belongings (water bowl, food bowl, bed, leash and collar or harness, toys etc.) in a big box and store it away for the time being.
. Talk about it.
. Write in a journal. Nobody has to know.
. Depending on your artistic talents, you could draw a picture of your pet, write a poem, create a scrapbook with memorabilia and pictures…
. Create a memorial in your garden or on your balcony.
12. How else can I get closure?
Another vastly personal topic. Although it is difficult to believe it at the time of euthanasia, time heals all wounds. Eventually, you will get over your sorrow.
Getting closure requires going through the flow of the various stages of grieving.
You can write a letter, like the one above about Jackie the kitty. After writing it, she said: “I still miss her, but I think writing this text has helped.”
Getting your pet’s ashes and “taking care of them” may also help with closure, as this typically happens after a week or so.
13. When should I get a new pet?
Most people recommend waiting until you achieve complete closure before getting a new pet. Adopting a new pet too soon may lead to bad decisions that you might regret, which is not fair to the new pet (or you and your family).
14. What do I tell my kids?
This is another very complicated topic. I would rather direct you to web sites (mentioned below) that explain things very well depending on the age of the child. You just don’t explain things to a 3 year old the same way as you would a 13 year old. There a re many things to be aware of. For example, it may be inappropriate to say that your pet “went to sleep” or was “put to sleep” and will never come back, as this may traumatize a child at bed time for years. After all, their buddy is never going to wake up…
16. How can I help my grieving elderly parents?
Again, a touchy topic… Sometimes, a pet is the last link an elderly person has to the world. If a grandma or grandpa cannot walk Fluffy in the neighborhood, a whole part of their social interactions may vanish all of a sudden.
I hope this helps you understand the process of euthanasia. In a sense, euthanasia is an act of love. You will rarely see it that way the day you lose your pet. But after your grieving period, I hope you will understand that you made the right decision.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
A LOOK BACK AT 2021…
A LOOK BACK AT 2021…
The beginning of a new year is a great time to reflect on past accomplishments. For me, as a surgeon, it includes thinking of all the patients we helped and which surgeries we performed the most.
This can give you an idea of which surgeries pets are most likely to need…
So here were our top 10 surgeries in 2021.
1. ACL SURGERY
It never fails.
ACL surgery remains the most common surgery we perform, mostly in dogs (and less so in cats).
We have different procedures in our toolbox depending on the patient.
. TPLO (Tibial Plateau Leveling Osteotomy) is THE most common surgery we perform, by far.
. The “traditional” technique with heavy nylon sutures can be used in well-selected dogs (and occasionally in cats).
. The TWO (Tibial Wedge Osteotomy) has come in handy a few times this year in dogs who had implants that prevented doing a TPLO, or who had extremely steep angle at the top of their shin bone.
. TTA (Tibial Tuberosity Advancement).
One size doesn’t fit all here. We don’t see every problem as a nail, and we don’t only have one hammer.
2. Mass removal
We’ve removed masses in and under the skin, in the chest, in the bone (legs, toes, jaws)…
Thankfully, not all tumors are cancerous, and we’ve removed many benign masses.
3. Belly surgery
Belly surgery or “exploratory laparotomy” allowed us to:
. remove foreign objects from the stomach
. remove body parts (gallbladder, spleen, adrenal gland)
. take biopsies
. remove bladder stones, etc.
You can read about bladder stone surgery here:

Some cats had their colon removed because of a serious condition called megacolon. This is the only definitive solution when cats are so severely constipated, that the colon has become a painful giant bag of dehydrated poop. At that stage, medications are a waste of time and money.
Procrastinating to move on with surgery invariably leads to a much worse anesthesia candidate. These cats may go from otherwise healthy to skinny and unhealthy. Not to mention the fact that they suffer from untreatable constipation.
We also performed a number of prophylactic gastropexies, a preventive procedure designed to present stomach twisting in dogs at risk for “bloat.” This life-saving procedure should be considered in Great Danes (the #1 breed for this disease), German shepherds, Labs and several other large dog breeds.
4. Joint dislocations
We’ve mostly treated joint dislocations in the hip and the knee. Some pets had trauma, others were born that way (congenital dislocation).
The most common one is the kneecap dislocation. The kneecap slides out of the groove where it is supposed to live, at the bottom of the thigh bone (or femur). It is common in dogs, and we’ve treated a few cats with that condition last year.
5. Fractures
We’ve fixed fractures in just about every bone this year, mostly the forearm (radius), the shin bone (tibia) and the thigh bone (femur), as well as some toes, the jaw and the arm (humerus).
To fix these broken bones, we’ve used plates and screws, pins, or a device called an external fixator.
Causes of broken bones mostly included jumping, falling or being hit by a car.
6. TECA
Total Ear Canal Ablation (TECA) is the only definitive treatment for dogs (most often Cockers) and cats who have never-ending ear infections. They lead to pain, head shyness and sometimes aggressiveness.
Unfortunately, most of these pets are treated with medications for years, which can’t even go down into the ear canal because it has become so swollen.
We occasionally perform a TECA in pets who had a tumor in the ear.
TECA is an invasive procedure, with possible complications, yet it fortunately works very well in the majority of patients.

7. FHO
FHO (Femoral Head Ostectomy) is used to treat hip dislocations or hip dysplasia.
The “ball” of the hip (femoral head) is removed during surgery.
FHO is also done in pets with a hip fracture or deterioration of the bone (e.g. Legg Perthes disease in small dogs).
8. Laryngeal paralysis
Dogs, mostly Labs, can have a condition that paralyzes their larynx, a.k.a. voice box, and causes them to suffocate. It’s an incredibly stressful condition. Fortunately, surgery (a “tie back”) allows them to have a wider airway, which typically works very well. These patients quickly go from suffocating to being able to breathe comfortably.
You can read about the amazing story of Mae Mae here:
9. Brachycephalic syndrome
This condition is seen in dogs (and rarely cats) with a flat face, which caused snoring and difficulty breathing: Bulldogs, pugs, Boston terriers, Persian cats etc.
It typically involves 4 conditions:
. The most visible part are stenotic nares (aka tiny nostrils) which prevents getting enough oxygen. Surgery involved making them wider, aka “a nose job” or a rhinoplasty.
. An elongated soft palate. The tip of the roof of the mouth is so long, that it covers the entrance of the windpipe. When it vibrates, it causes snoring. We can shorten it during surgery.
. Saccules are fleshy structures at the beginning of the windpipe. Over time, the saccules can pop out into the airway – and further block the flow of oxygen. We can remove them during surgery.
. A tiny windpipe, which we can’t do anything about.
You can read more about this surgery done on Kasper here:
https://www.drphilzeltzman.com/blog/guess-who-had-a-nose-job-today/
10. Reconstructive surgery
We did multiple surgeries that required reconstructing a body part:
. Cleft palate (or roof of the mouth), which you can read more about here:
https://www.drphilzeltzman.com/blog/squirrel-gets-a-new-lease-on-life-after-cleft-palate-surgery/
. Male cats who could not pee (P/U or perineal urethrostomy).
. A dog’s penis which had a (benign) tumor.
. Hernias, which are a condition where an organ ends up where it shouldn’t be.
Remembering some of the surgeries we’ve performed in 2021 is also an opportunity to give credit to the wonderful vets, nurses, and pet owners who have been caring for them.
Until next time,
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Ninja, my biggest surgical & ethical challenge in 2021
“I beg you for help.”
Such was the subject line of the email.

In the email, a pet owner explained:
“My dog Ninja, a 6 year old Siberian Husky, just had a CAT scan, then surgery to drain a cyst in his enlarged prostate” (17 cm long – about 7 inches).
“Because of the pressure on the colon and the bladder, Ninja couldn’t defecate or urinate!”
“His bladder has been so over-stretched, that it couldn’t contract and now Ninja still can’t urinate. A urinary catheter was placed temporarily… and the only option the surgeon gave us was euthanasia!”
“I don’t want to put him down. He is eating, drinking and (now) pooping. He acts normal but can’t pee. Please help me, I am very desperate.”
Desperate times call for desperate measures.
Ninja had a condition similar to unfortunate older gentlemen who struggle to pee because of an enlarged prostate. It is a frustrating & painful situation. But in a dog, it can be life-threatening.
There is a better solution than euthanasia. I suggested a surgery that involves placing a special tube in the bladder and allows draining the bladder on demand.
It’s certainly not for every pet owner, but Ninja’s owners were exactly the right people for the challenge: dedicated, attentive, and totally in tune with their dog. They had done their homework and found out about this option by reading my blog about Madeline, who had the same surgery for a different problem (a bladder tumor).
Chapter 1
Time was of the essence, so we quickly scheduled surgery at Brodheadvsille Vet Clinic.
Ninja had a “cystostomy” surgery, where a tube was placed to drain the bladder through an opening in the skin.
In addition, Ninja was neutered. After that necessary step, male hormones would decrease and cause the prostate to shrink. That would reduce the pressure on the urethra and allow Ninja to urinate.
Chapter 2
Everything went according to plan for about a month… until Ninja accidentally stepped on the tube.
The logical next step was to replace the life-saving drain. Unfortunately, preop bloodwork showed some concerning changes. Ninja’s immune system was attacking his own red blood cells (hemolytic anemia) and platelets (thrombocytopenia). This double condition is called Evans’ syndrome.
So we changed plans. Since it was too risky to perform surgery with such low numbers of red blood cells and platelets, we placed a traditional urinary catheter to allow Ninja to urinate.
We were able to do this thanks to the generosity of another practice owner near Allentown, PA.
The catheter had to be changed frequently to lower the risk of bladder infection (UTI).
His faithful owners would drain the bladder multiple times a day to allow it to stay small. Remember, the bladder was so over-stretched, that it couldn’t contract anymore…

Chapter 3
At that point, Ninja was referred to a board-certified internist (a medicine specialist) to manage his Evans syndrome.
Meanwhile, Ninja still couldn’t pee!
To make matters worse, an ultrasound showed that the prostate now had an abscess. Again, euthanasia was recommended.
Again, his owner called me to see if there were any other options.
After reaching out to multiple specialists, we found one willing to help. My amazing nurse and I suggested a completely crazy plan:
. An ICU specialist at a specialty hospital in NJ accepted to let us use the key to our problem: a special transfusion with platelets to help with clotting.
. We would drain the abscess at another practice in NJ, and place a new cystostomy tube to allow Ninja to pee.
. We would recover Ninja under the supervision the ICU specialist.
Amazingly, Ninja’s owners decided to go with surgery, about 2 months after the first one.
The procedure was uneventful, and after 2 days in ICU, Ninja went home.
Then came weeks and months of amazing dedication from Ninja’s owners.
Long story short, Ninja progressively got better and stronger.
Then out of the blue, to everybody’s surprise, he started to pee on his own!
After agonizing over the right time to remove the tube, we eventually did, once we were convinced that Ninja was emptying his bladder on his own sufficiently to survive.
Now you understand why Ninja was such a technical and mostly ethical dilemma for me.
When should a surgeon stop helping?
When should a pet owner stop hoping?
When should a pet to cross the rainbow bridge?
Why did I choose Ninja’s story…
… over so many other amazing pet stories I was fortunate to play a part in in 2021?
Because of the number of people who played a role in Ninja’s survival.
In the middle of the COVID crisis, it was an absolutely astonishing display of generosity, love and care, by multiple vets and nurses.
Across half a dozen practices.
And across 2 States (PA & NJ).
(trust me, I gave you the short version!!!)
Everybody rallied behind Ninja, led by his loving owners.
And the result is one happy, playful, fluffy Husky, whose only wish is to be comfortable, to be able to pee, and to return his owners’ love.
Ninja’s owner created an amazing video summary.
It’s a story about the love of a family pet.
A story about the power of dedication.
A story about not taking no for an answer.
You can watch it here: https://vm.tiktok.com/ZMRatj6Co/
Fair warning: it’s a tiny bit emotional…
What’s the moral of the story?
1. Neutering early in life decreases or eliminates the chances of having prostate issues in male dogs. There are many other good reasons, which you can read about here:
https://www.drphilzeltzman.com/blog/top-10-reasons-to-neuter-your-pet/
2. You are your pet’s best advocate. If something makes no sense to you, don’t give up. Sadly, there is not a solution or a cure for every condition. But at least, you should explore your options.
Don’t take no for an answer. Get a second opinion.
This is exactly what Madeline’s and Ninja’s owners did. They didn’t take no for an answer, and they saved their dogs’ lives.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
E Collars and Your Pet- Cone of Shame or Best Friend?
Ah, the dreaded “cone of shame…”
After any surgery, we strive to send your pet home with an incision that looks as nice as possible. The plastic cone or E collar (short for Elizabethan collar) was created to prevent licking. Without it, licking or chewing can cause irritation and discomfort.

At best, that may leave a hairless, discolored, ugly scar – for life.
Or it could lead to an open incision, that needs another surgery to close it up.
At worst, it can cause a serious infection.
| WARNING: some pictures below might be disturbing to some sensitive readers. |
Despite the stubborn urban legend that animal saliva speeds up healing, licking an incision is a sure way to slow down healing. The tongue, especially in cats, is so rough, that it can destroy healing tissue, and therefore delay healing.
Depending on the particular pet or level of discomfort, licking can lead to nibbling and chewing, especially when nobody is around to watch or distract them.
Pets have an amazing inherited skill, which allows them to chew up twenty stitches or staples in less than two seconds flat. By the time you realize it, it’s too late!
Below is an example of a dog who was caught in the act. She went home with a cone that is too short, and does not prevent reaching the incision. Clearly, the correct fit is critical.

I cannot begin to count how many times pet owners have asked me if their pet really has to wear an E collar.
And I cannot begin to tell you how many clients thought their pet was different, or well-behaved, or well-trained, or smarter, and didn’t need a cone.
Or how many pet owners were in tears after their pet chewed the incision open after they removed the cone “for only 5 minutes” or “just to give him a break” or “because she looked so sad.”
Below is a (mild) example of what happens when a pet licks the incision.

I cannot begin to add up all the extra money owners have paid to fix open incisions at their vet or the emergency clinic.
And I cannot tell you how many clients swear that they will not leave their pet’s side for 2 or 3 weeks. Meanwhile, I’m pretty convinced that these clients will need to sleep, or go to the bathroom, or get a bite to eat. There is no such thing as 24/7 supervision with a pet!
Depending on how bad the damage is, treatment may require rinsing the open area, cutting out damaged tissue and re-stitching the entire incision. For a little bit of perceived freedom from the evil cone, clients sometimes end up spending more money in anesthesia, surgery and antibiotics to fix an entirely avoidable problem, not to mention the discomfort the pet goes through – and a longer recovery. And ironically, then the pet needs a cone for even longer!
Below is another (mild) example of what happens when a pet licks the incision.

Leaving the E collar on at all times is the best way to get your pet used to it. If you feel bad for your pet and take the cone off, then put it back on when you leave, your pet may take it as a punishment and may try to remove or destroy it.
Patients can absolutely eat, drink, walk, pee, poop, and sleep with a cone on. In fact, the stricter you are with the cone, the quicker they will get used to it. In addition, pets do not hold grudges, so they will not be mad at you for being strict with the rules.
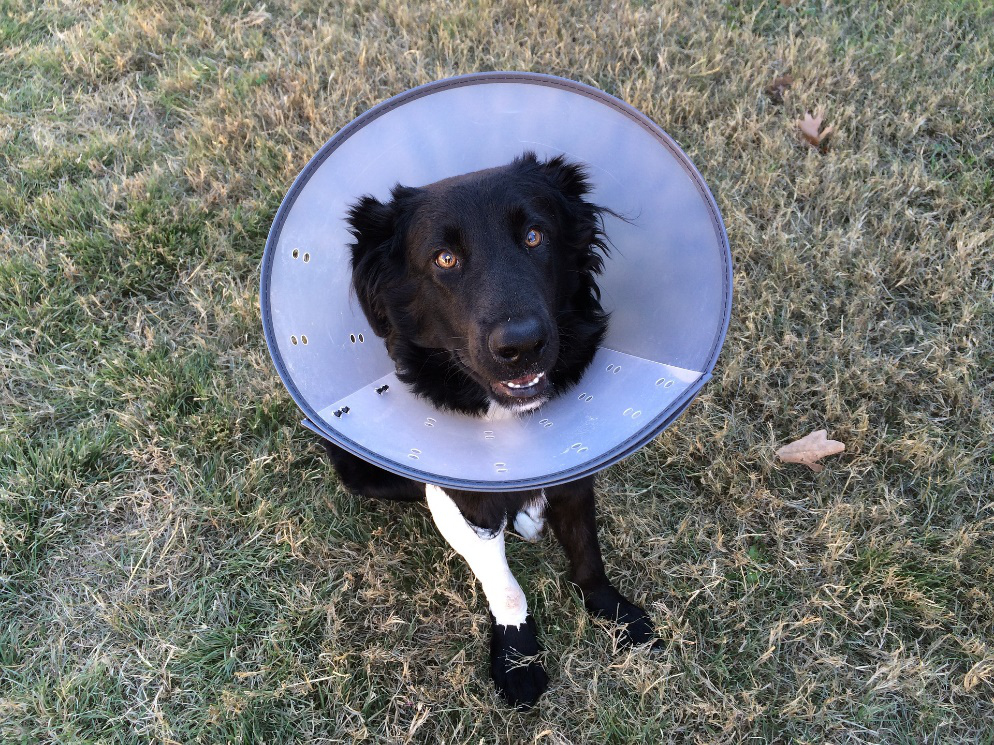
Collars are not to “shame” pets or annoy owners, they are essential for quicker and better healing of the incision. Call it a necessary evil or a cheap insurance policy. Next time your vet recommends an E collar or a similar device, please follow their advice. It truly is in your pet’s best interest.
Moral of the story?
The plastic cone is your pet’s best friend.
Any surgery has complications. Some are not predictable. Licking an incision is totally avoidable. We know how to prevent that. Please trust us, and please be part of the solution.
Your pet, in the end, will thank you for it.
What about alternatives to the plastic cone?
Marketers spend a fortune trying to convince pet owners that their alternative is better than the hard plastic cone.
There are soft cones, hard cylinders, foam “donuts,” inflatable “donuts,” various covers and sleeves and more.
As a surgeon, I have witnessed what seems like every conceivable complication.
Experience has shown me that these options are not as fool-proof as the standard plastic cone.
A stubborn or itchy pet will lick around a donut or soft collar, we see it all the time!
Bitter Apple or similar product may be placed around the incision – not directly on it. However, this does not deter some pets at all. Some actually love the taste!
So again, the hard plastic cone is your pet’s best friend… and the cheapest insurance policy against licking.
Phil Zeltzman, DVM, DACVS, CVJ, FF certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!
Should you wait to get help for your pet?

Your pet is vomiting. Should you wait to go to the vet?
Your pet is limping. Should you wait to seek help?
Your pet has a mass. Should you wait to have it looked at?
These are common dilemmas, and the answer is… it depends!
Let’s keep our 3 examples.
. Many pets vomit every once in a while, and they are perfectly healthy otherwise.
Other times, repeated vomiting is a sign that something is brewing inside. And it could be anything: stomach problems, intestinal conditions, kidney disease, cancer etc.
. Some pets limp because of a sprain and get over it by the next day, just like a human.
Other times, ongoing limping is a sign of a problem: elbow arthritis, hip dysplasia or the most common cause of limping: a torn ACL.
. Many pets have skin masses. Most masses can only do one thing: get bigger. Very rarely does a mass get smaller. It would defy science: as cells divide, which they are genetically programmed to do, the mass gets bigger. It can be slow or it can be fast, but they usually get bigger over time. The only way to objectively know what is going on is to measure it.
So what’s a pet lover to do?
Should you keep an eye on it?
For a short while, possibly.
Waiting any longer is rarely a good idea.
. Repeated vomiting can lead to dehydration and electrolytes imbalances.
. An untreated joint problem invariably leads to arthritis, which can only get worse over time.
. A small mass is easier, less invasive and cheaper to remove than a large mass. This translates to longer anesthesia, higher surgery fees and higher chances of complications.
Occasionally, you will be a bit early and it’s a false alarm.
Most times, you will be right and acting early will save you time, money and frustration while avoiding pain for your pet.
At the very least, call your vet to ask questions. Many vets now offer telemedicine consultations, which means you don’t even have to take your pet to the vet. You can get advice from the comfort of your home.
Just keep in mind that vomiting may require X-rays or an ultrasound, limping may require X-rays and a mass may require lab testing.
Either way, don’t procrastinate, it rarely leads to good results.
Phil Zeltzman, DVM, DACVS, CVJ, Fear Free Certified

Dr. Phil Zeltzman is a traveling veterinary surgeon in Pennsylvania & New Jersey. An award-winning author, he loves to share his adventures in practice along with information about vet medicine and surgery that can really help your pets. Dr. Zeltzman specializes in orthopedic, neurologic, cancer, and soft tissue surgeries for dogs, cats, and small exotics. By working with local family vets, he offers the best surgical care, safest anesthesia, and utmost pain management to all his patients. Sign up to get an email when he updates his blog, and follow him on Facebook, too!

